Table of Contents
Adolescent Mental Health: A National Emergency
Written By: Charlie Health Editorial Team
October 27, 2021
6 min.
A National State of Emergency in Child and Adolescent Mental Health was declared last week by a consortium of leading medical professionals, including the American Academy of Pediatrics, the American Academy of Child and Adolescent Psychiatry, and the Children’s Hospital Association. In a series of stark findings and vehement recommendations for policymakers, the group of mental health providers cited the reasons for their declaration as “soaring rates of depression, anxiety, trauma, loneliness, and suicidality that will have lasting impacts on [youth], their families, and their communities.”
Learn more about our Clinical Review Process
Table of Contents
A National State of Emergency in Child and Adolescent Mental Health was declared last week by a consortium of leading medical professionals, including the American Academy of Pediatrics, the American Academy of Child and Adolescent Psychiatry, and the Children’s Hospital Association. In a series of stark findings and vehement recommendations for policymakers, the group of mental health providers cited the reasons for their declaration as “soaring rates of depression, anxiety, trauma, loneliness, and suicidality that will have lasting impacts on [youth], their families, and their communities.”
As providers of teen and young adult mental health care, Charlie Health’s clinical team recognizes the challenges facing our youth––the effects of COVID-19 on youth mental health; the suicide crisis facing kids and teens; and the collective trauma of both the pandemic and other world news of the past two years. In short, this declaration comes as no surprise to our team; the state of youth mental health and youth mental health care are emergencies. Charlie Health provides solutions for high-acuity patients and families every day through virtual intensive outpatient programming, many of whom cited exorbitant wait times, inaccessible costs, and a lack of personalized treatment in mental healthcare throughout the US while searching for appropriate treatment options.
Barriers to care
The barriers to entry for mental healthcare are even higher for communities of color, rural communities, and LGBTQIA+ youth. The National State of Emergency acknowledges this as well, citing not just the impacts of COVID-19 on communities of color and other minority groups, but also the health disparities resulting from structural racism. These disparities of course extend to youth and families who live too far away from acute mental healthcare providers, who cannot afford traditional intensive outpatient programs, and youth who face discrimination and erasure in accessing healthcare based on their gender and/or sexuality.
Solutions to the crisis
There are solutions though, as outlined by the consortium. One of the most important ways policymakers can improve the current youth mental health crisis is by increasing access to programs that work directly with the most vulnerable, high acuity patients (as our Chief Clinical Officer, Dr. Caroline Fenkel, has discussed). The National State of Emergency’s policy suggestions say as much:
“[Policies must] address the ongoing challenges of the acute care needs of children and adolescents, including shortage of beds and emergency room boarding by expanding access to step-down programs from inpatient units, short-stay stabilization units, and community-based response teams.”
At Charlie Health, we also believe that addressing the gap in the continuum of care for youth and their families who need a higher level of mental health care requires innovative solutions. One of them is expanding access to virtual intensive outpatient programs. We are passionate and determined to address these crises with the utmost care, leading clinical expertise, and a personalized approach to enhance patient experience.
How IOP can help
Do you need more support with
your mental health?
Charlie Health can help.
Charlie Health provides mental health treatment programs, IOPs, for youth in need of more than one-time-per-week therapy. IOPs are a clinically appropriate step-down program for those discharging from inpatient or residential care. Alternatively, many youth who were seeing a therapist on a weekly or biweekly basis enroll in IOP when mental health symptoms progress, and a higher level of care is needed. In this case, Charlie Health’s IOP serves as a preventative mental health care solution, allowing patients to receive comprehensive care from home and preventing a mental health crisis which could result in an admission to the emergency department. The goal is to meet patients and families where they are, with accessible care that provides sustainable healing for high-acuity patients.
There is federal support for our commitment to tackle the youth mental health crisis head on, as well. In a report released by the US Department of Education earlier this month addressing how schools can better address mental health challenges faced by students, the DOE emphasized how the COVID-19 pandemic has only “intensified” the mental health crises that has been mounting throughout the crisis.
What else can be done?
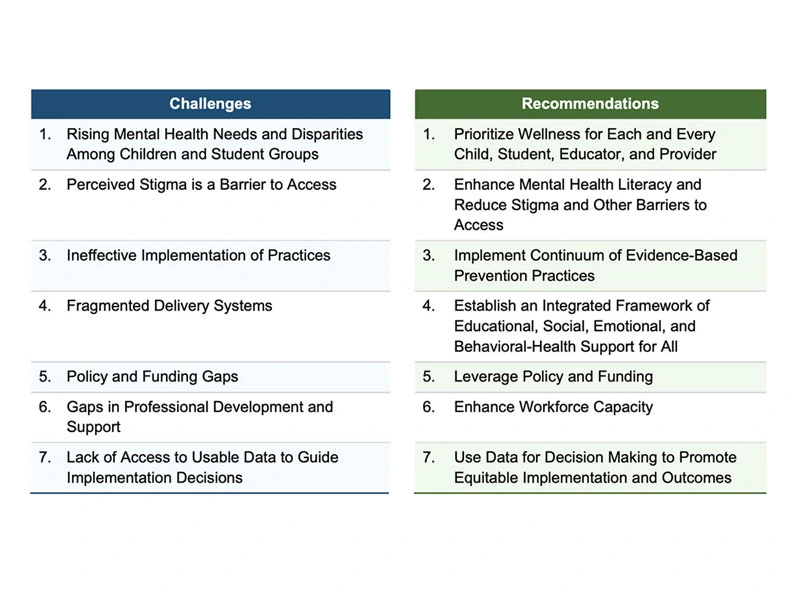
The DOE identified seven key challenges facing youth mental healthcare in the US, along with seven corresponding policy recommendations:
The broader youth mental health crisis
According to the report–and in line with data we’ve sourced before––the Department of Education reported that:
- In a survey conducted in April and May 2020, one in four youth (ages 13–19) reported an “increase in sleep loss due to worry, feeling unhappy or depressed, feeling constantly under strain, and loss of confidence in themselves.” (Margolius et al., 2020).
- A CDC report found one quarter of respondents ages 18–24 had contemplated suicide in the 30 days prior to completing the survey (Czeisler et al., 2020).
Pediatricians in Washington State are reporting: - Significant increases in youth with eating disorders, anxiety, mood disorders and depression with suicidal thoughts and self-harm behaviors (nearly twice the rate of adults over 40).
- Families experiencing long wait times and limited access to mental health services.
- LGBTQIA+ youth are having specific challenges navigating limited social support when affirmation and support are particularly important, resulting in sleep disturbances, decreased physical activity leading to unhealthy weight gain, and abuse of substances.
- A significant number of previously stable youth have experienced new-onset or exacerbated eating disorders, depression, with some requiring increased use of medications, hospitalization, or other higher levels of care.
When leaders in both medicine and government policy align for a shared goal, we know it is time to double down on our work and goals. Charlie Health continues to expand services across the US, providing critical solutions to thousands of families. But there is still work to do. We need to continue to educate policy leaders, healthcare professionals, parents, teachers, community leaders, and youth themselves about available resources and how to find appropriate support when you need it most. As a first-of-its-kind provider of virtual intensive outpatient programs for teens and young adults, Charlie Health is committed to both adherence with and the continued innovation of mental health progress. We don’t want to just treat the mental health issues surging among adolescents and young adults–we want to address the root causes ranging from school resources to family communication to financial barriers.
At Charlie Health, our goal is to ensure the effective delivery of care for all clients. As such, we are unable to accept clients with any eating disorder as a primary diagnosis at this time.
Teen and young adult IOP at Charlie Health
If you or a loved one is struggling with mental health, know that you are not alone. Youth across the country are facing unprecedented challenges and it’s more important than ever to support yourself and those around you in reaching out for help. It’s our mission at Charlie Health to help as many youth and families as possible achieve sustainable healing through accessible and personalized treatment programs that meet their unique needs and goals. Contact us today to speak with our Admissions Team who can support you in navigating which treatment options may be right for you, and how to get started.