
Table of Contents
New Research: Virtual Intensive Outpatient Care Improves Teen Mental Health

Written By: Dr. Kate Gliske
November 15, 2022
5 min.
New peer-reviewed study finds that Charlie Heath’s telehealth program improves access and outcomes for teens and young adults in crisis.
Learn more about our Clinical Review Process
Table of Contents
The United States is currently facing a youth mental health crisis. Nearly half of U.S. high schoolers report feeling persistently sad or hopeless, and suicide is now the second leading cause of death among young people. The situation is particularly pronounced among certain demographics. For example, nearly half of LGBTQIA+ youth seriously considered suicide in the past year (compared to 1 in 5 teens overall) and low-income teens are more likely to be prescribed potentially unnecessary antipsychotic drugs than their higher-income peers.

What if healing could happen at home?
If you or someone you love is struggling with their mental health, don’t wait to get help. Fill out our form to learn if Charlie Health is right for you.
Consequences of untreated health conditions
When left untreated, mental illness can have both short-term and long-term consequences for teens and young adults. In addition to impacting a person’s mental and physical wellbeing, it can lead to school dropout, unemployment, substance abuse, self-harm, violence, and even death.
We know that timely access to effective treatment is critical to care, yet young people and families continue to face a shortage of services. Research shows that 122 million Americans lack treatment options for young people with serious mental health issues, with the greatest gaps in care seen in rural communities. Emergency rooms across the country continue to fall short on the beds and providers needed to meet the needs of suicidal adolescents. And even if there is a psychiatrist or therapist in your area, it might be difficult to find someone who looks like you or shares the same cultural experiences.
All of this paints a grim picture, showing that less than half of teens and young adults with a mental health diagnosis receive the treatment they need.
But what about telehealth?
Although telehealth has been used for more than a decade, it wasn’t widely adopted until the COVID-19 pandemic forced professionals across the healthcare industry to bring their services online in order to connect with their clients.
For Charlie Health and others in the world of youth mental health, telehealth has long held a clear place in addressing the shortage of mental health services for those with severe needs. However, there was still debate over whether virtual intensive outpatient programs (IOP) could eliminate certain limitations associated with in-person care while yielding equal outcomes upon discharge.
Previous research comparing IOP outcomes by insurance type—meaning public insurance (e.g., Medicaid) versus private insurance (e.g., commercial)—found disparities among teens for both virtual and in-person settings. A shortage of providers and lengthy appointment wait times were other problems associated with traditional, in-person care—a problem for teens and young adults who require more comprehensive treatment than once-weekly therapy. Transportation and other accessibility concerns have also been found to make in-person intensive outpatient treatment less effective. To further understand the potential benefits of telehealth for teens and young adults with mental health conditions, we needed more research on the clinical and engagement outcomes.
A look at the research
Led by Dr. Caroline Fenkel DSW, LCSW, Co-Founder and Chief Clinical Officer at Charlie Health, and Dr. Kate Gliske, Director of Research & Clinical Outcomes, the team researched the following questions:
- Does personalized telehealth lead to improved clinical outcomes and engagement for teens and young adults attending a remote Intensive Outpatient Program (IOP)?
- Do the outcomes vary based on identifying factors such as insurance status or gender identity?
In partnership with Dr. Phyllis Solomon, Professor of Social Work at the University of Pennsylvania, Fenkel and Gliske studied mental health outcomes for 495 youth who were enrolled in Charlie Health’s IOP over the course of nine months. All participants were based in 14 states, participated in seven or more treatment sessions, and completed both intake and discharge surveys between July 2021 and April 2022. Importantly, approximately three-fourths of youth had private insurance while the remaining 24% had public insurance—a ratio which mirrors the national trend for individuals under age 65.
Using this data, as well as additional self-reported intake surveys and discharge assessments, the researchers analyzed program attendance and symptoms related to depression, suicidal ideation, and self-harm.
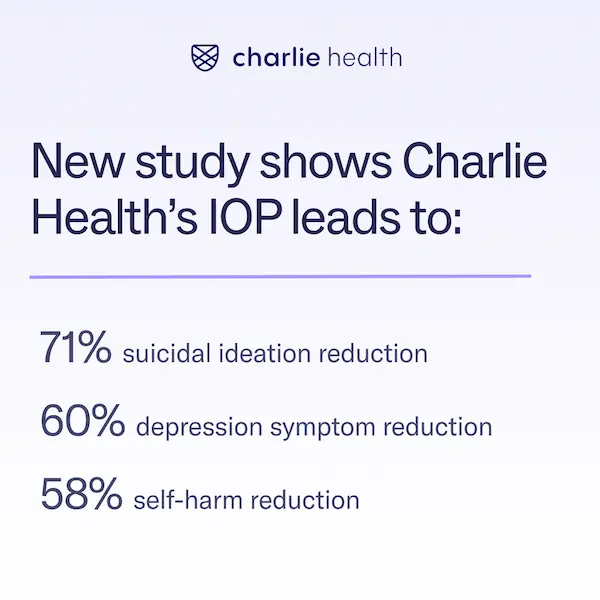
So, what did they find? The headline is that virtual care has the potential to play a significant role in addressing the youth mental health crisis, but more specifically the study found that:
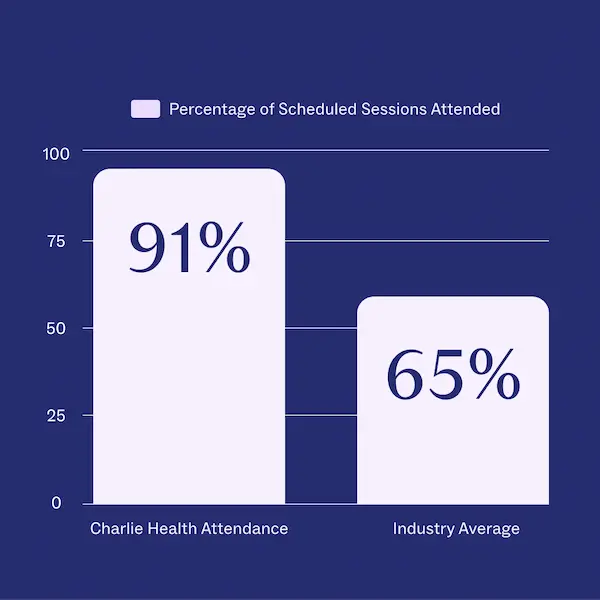
- Teens and young adults who received treatment via Charlie Health’s virtual IOP attended 91% of scheduled sessions (compared to a 65% industry average). This was true across all genders, with nearly a quarter of teens self−identifying as a gender other than male or female, and 20% self−identifying as transgender.
- Participants reported significantly fewer depressive symptoms (60%).
- More than half of all participants who had self-reported self-harm behaviors upon starting Charlie Health’s IOP were no longer self harming at discharge.
- Of youth who reported active suicidal ideation at intake, 71% were no longer suicidal post-discharge.
- There were no significant differences or reductions in clinical outcomes (such as depression and suicidal ideation) between those with public and private health insurance.
A solution for increasing access to mental health services
The research concluded that virtual treatment programs have the potential to meet the growing demand for greater access to behavioral health services for young people. By providing care via telehealth, such as with Charlie Health’s virtual intensive outpatient program, teens have an opportunity to receive treatment without many of the traditional limitations of in-person care—including location, transportation, and insurance type. “Charlie Health is fundamentally shifting the conversation around virtual therapy and mending fractures in the system, one client at a time,” wrote Dr. Fenkel.
“With significant improvements to access and measurable improvements in outcomes, we are revolutionizing life-saving care for young people who need it most,” Dr. Caroline Fenkel
Charlie Health focuses on this systemic change by increasing access to trauma-informed, evidence-based care that is focused on helping teens to process intense emotions and work through challenges. Practices like cognitive behavioral therapy (CBT) and dialectical behavioral therapy (DBT) skills focus on identifying negative thoughts and behavior patterns, then working with a therapist to develop the skills to cope with these problems. Charlie Health’s personalized mental healthcare programs are rooted in group sessions, which can help teenagers form meaningful connections with their peers and empower teens to make positive changes—regardless of where they live or who they are.
Get help today
If you or someone you know might benefit from a higher level of mental healthcare, Charlie Health is here to help. Founded in 2020, Charlie Health is the largest virtual mental health clinic for teens and young adults who are struggling with serious mental health disorders. Our personalized Intensive Outpatient Programming (IOP) consists of support groups, individual therapy, and family therapy in order to best meet the needs of each person.
Whether you’re exploring treatment options for the first time or searching for extra support, Charlie Health provides individualized and evidence-based mental health care in a safe, supportive space.
Contact Charlie Health to learn more today.
References
https://www.hhs.gov/sites/default/files/surgeon-general-youth-mental-health-advisory.pdf
https://www.cdc.gov/mmwr/volumes/71/su/su7103a3.htm
https://www.thetrevorproject.org/survey-2022/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3731155/
https://pubmed.ncbi.nlm.nih.gov/24233052/
https://www.charliehealth.com/areas-of-care/depression
https://www.charliehealth.com/areas-of-care/self-harm
https://www.charliehealth.com/post/what-is-the-difference-between-cbt-and-dbt-therapy
https://www.charliehealth.com/post/why-your-teen-should-enroll-in-group-therapy




