Table of Contents
Racism is a Form of Trauma
Written By: Charlie Health Editorial Team
February 18, 2023
5 min.
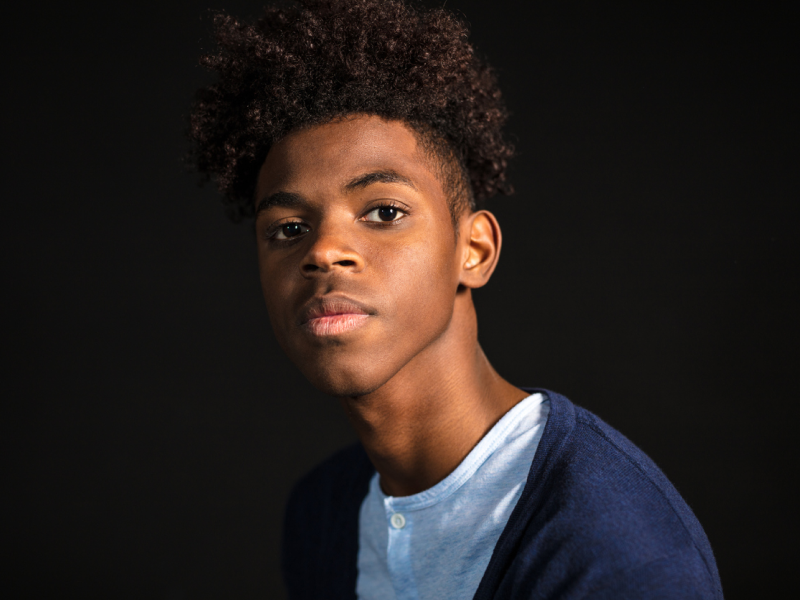
Understanding the mental health effects of racism as a form of trauma is critical for creating safe and inclusive spaces and promoting healing and recovery for BIPOC teens, young adults, and families.
Learn more about our Clinical Review Process
Table of Contents
We also know that racism is a mental health issue that plays a significant role in the youth mental health crisis. What not enough people understand, though, is that racism doesn’t only exacerbate trauma—it also is trauma, in and of itself. Here’s what the field of mental health understands about racial trauma, what it gets wrong, and where we need to go from here.
What is racism?
Abolitionist activist and scholar Ruth Wilson Gilmore, PhD defines racism as “the state-sanctioned and/or extralegal production and exploitation of group-differentiated vulnerability to premature death.”
Racism, like any form of oppression, may be ideological (a belief system), institutional (built into institutions), interpersonal (privileging one group over another), and/or internalized (self-directed).
What is trauma?
Trauma refers to the range of emotional responses that many people experience after a major adverse event. Common examples of traumatic events, using the standard definition, include sexual assault, include intimate partner violence, accidents, and natural disasters.
What is racial trauma?
According to an article in PTSD Quarterly, racial trauma can be defined as “the cumulative traumatizing impact of racism on a racialized individual, which can include individual acts of racial discrimination combined with systemic racism, and typically includes historical, cultural, and community trauma as well.”
Where the research stands on racial trauma
While research isn’t necessary to acknowledge the clear associations between racism and trauma, some experts have developed ways of conceptualizing the relationship.
In 2002, Hugh F. Butts, MD published the first critique of racial discrimination’s exclusion from the diagnostic criteria for post traumatic stress disorder (PTSD) in The Diagnostic and Statistical Manual of Mental Disorders (DSM). “Even in those instances in which African-Americans are objects of discrimination and describe symptoms consistent with PTSD,” Dr. Butts wrote, “their symptoms may be dismissed or trivialized because of the view that the stressors are not catastrophic enough … to warrant a diagnosis of PTSD.”
Despite Dr. Butts’ scathing and deserved critique—as well as the compilation of case studies in Dr. Butts’ paper and countless studies published by other authors—race-based trauma is still left out of the official PTSD diagnosis more than 20 years later.
Join the Charlie Health Library
Get mental health updates, research, insights, and resources directly to your inbox.
You can unsubscribe anytime.
In another study, 71% of therapists surveyed reported working with patients who experienced race-based trauma. The survey used, the Race-Based Trauma Survey for Counselors, is one of several instruments experts have designed to understand and measure the impact of race-based trauma. Others include the Race-Based Traumatic Stress Symptom Scale and the Race-Related Stressor Scale for Asian American Vietnam Veterans.
Where the mental health field falls short
The trivialization and limited exploration of race-based trauma have caused significant challenges in the broader mental health field’s understanding of the unique form of trauma. Here are a few examples of how this plays out:
- There is very little research looking into treatment for PTSD and race-based trauma, and no professional recommendations for treatment.
- There is no existing training, to our knowledge, to help therapists identify and treat race-based trauma.
- The underrepresentation of people of color in clinical trials leads to underrepresentation in PTSD medication research.
- Over 86% of psychologists and therapists are white, meaning the vast majority of mental health professionals need training and guidelines to appropriately serve patients of color who have experienced race-based trauma.
Do you need more support with
your mental health?
Charlie Health can help.
Where we need to go from here
In order to support the mental health and well-being of people with race-based trauma, we need to:
Advocate for the inclusion of race-based trauma in the definition of PTSD
The DSM has made significant changes before in service of equity and justice. For example, in 2013, the DSM contributed to ending the pathologization of transgender identity by replacing an offensive and nonscientific diagnosis with “gender dysphoria.” In 1973, “homosexuality” as a disorder was removed.
Additionally, with new editions and updates to existing editions coming out every few years, there’s ample opportunity for PTSD’s expansion to include race-based trauma.
Why does the DSM diagnosis matter? While a diagnosis is sometimes nothing more than a code for insurance companies or a starting point for treatment, equity-focused shifts in terminology and definitions can have ripple effects like increased legitimacy and awareness and validation of people’s experiences.

Advance the clinical understanding of race-based trauma
Among adult populations, mental health clinicians and researchers need to become more aware of race-based trauma identification and treatment—and invest more time and money into dedicated research pursuits.
Increasing our knowledge also demands a better understanding of the unique impact on children, adolescents, and young adults. Researchers Farzana Saleem, PhD, Riana Anderson, Ph.D., and Monnica Williams, Ph.D. have greatly contributed to the body of literature on this topic. In 2020, they developed a conceptual model for addressing race-based trauma in young people specifically.
Partner with community leaders to make clinical trials feel safer for people of color
Clinical trials for psychiatric medication are important in developing more and better treatments for PTSD and other mental health challenges that may reduce quality of life. However, due to medical distrust, flawed recruitment methods, and a host of other factors, there is an underrepresentation of people of color in clinical trials. Testing new medications in majority white populations, which public health institutions can partner with community leaders to co-create strategies that make people with medical distrust feel safer in clinical trials and other medical settings.
Make it easier for people of color to find and become mental health professionals
“With the resurgence of political and racial tension against people of color, finding a therapist to help young people show up authentically in the therapeutic space has become even more critical,” wrote Chelsi Clark Ph.D., NCSP, LPC, Charlie Health’s Director of BIPOC Programming. “The history of oppression and racism is connected to the current circumstances of the deteriorating mental health of Black and brown youth.”
Ensuring everyone can access racially concordant mental health professionals requires more therapists of color. We need more programs like the Minority Fellowship Program that reduce financial barriers to education and training.
BIPOC Programming at Charlie Health
The importance of BIPOC clinical programming at Charlie Health's IOP for teens, young adults, and families cannot be overstated. By providing culturally-sensitive and responsive care, Charlie Health's BIPOC clinical programming can help improve outcomes and increase access to mental healthcare for BIPOC teens and young adults. The integration of BIPOC clinical programming within Charlie Health's IOP can also help to address disparities in mental health care for BIPOC populations and promote equity in access to care. To learn more or get started, reach out today.





