
Table of Contents
How Charlie Health Supports Clients With Substance Use Disorder

Written By: Elizabeth Kroll

Clinically Reviewed By: Claire Streeter
July 23, 2024
5 min.
Learn about how our specialized intensive services support the well-being of clients with substance use disorder.
Learn more about our Clinical Review Process
Table of Contents
In 2022, over 100,000 people died from a drug-involved overdose. Since 2015, the United States has seen a 105% increase in drug overdose deaths, and the rates continue to rise. While non-prescribed or illicit substance use used to be treated as a medical disease, over the past 20 years or so, the narrative of addiction treatment has shifted. Instead, experts have understood substance use disorder (SUD) to be both a medical and behavioral health issue, and providers have started to acknowledge the underlying causes of addiction, such as trauma or co-occurring mental health disorders.
At Charlie Health, we offer a SUD track that recognizes the holistic approach needed when treating addiction. This specialized treatment option offers a space for clients to work through underlying mental health concerns while getting support for reducing their substance usage (meaning illicit and non-prescribed substances). Keep reading to learn how Charlie Health supports clients with SUD and the outcomes of clients who receive specialized SUD treatment with us.

We specialize in supporting people with substance use disorder
Intensive virtual care for people with serious mental health conditions.
Substance use prevalence in the United States
The Substance Abuse and Mental Health Administration (SAMHA) is a government agency tasked with collecting data on rates of substance use and behavioral health. Data from their 2022 report indicated that about one-quarter (24.9%) of people over the age of 12 had used illicit drugs within the past year. These illicit drugs could include marijuana (including smoking, vaping, and other modes of use), cocaine (including crack), heroin, hallucinogens, inhalants, and methamphetamine, as well as the misuse of prescription stimulants, tranquilizers, sedatives, and pain relievers. When broken down into more specific age groups, they found that young adults between the ages of 18-25 were the most likely to be using illicit drugs, with almost half of respondents indicating that they’d used at least one of the previously mentioned substances within the last year.
While the overall usage of these substances can be concerning on its own, just using a substance once does not automatically indicate a SUD. According to SAMHA, approximately 9.7% of the US population over the age of 12 had a diagnosed drug use disorder, with the percentage being highest for 18-25 year-olds at 18.6%. Rates of SUD diagnoses also differed between different races, with Native Americans having the highest rates at 17.3% and Asian Americans having the lowest rates at 4.9%. However, it is important to note that drug use is often underreported due to the stigma that surrounds it, therefore, the actual rates of drug use disorders are most likely higher than we know.
Substance use and mental health
Substance use disorders have a high comorbidity rate with other mental health concerns, including anxiety, depression, bipolar disorder, ADHD, and borderline personality disorder. According to the National Institute on Drug Abuse, over 60% of adolescents in treatment for a substance use disorder could be diagnosed with another mental illness. SAMHA also reports that adolescents who experienced a major depressive episode were more likely to have used substances in the past year compared to their counterparts who had not experienced a major depressive episode. The status with adults gets more specific, finding that adults with a mental illness were more likely to be users of illicit drugs. These rates of overlap between SUDs and mental health disorders only further drive home the point that they must be treated together.
Charlie Health’s substance use disorder treatment
Clients at Charlie Health who take part in our SUD track are offered a myriad of resources to support them with their substance use as well as their mental health. They are offered education on the biological, psychological, and social aspects of addiction. Our evidence-based treatment model takes an interdisciplinary approach, integrating knowledge from cognitive-behavioral therapy (CBT), motivational interviewing, family dynamics, and others. Overall, we emphasize the importance of assessing and improving a client’s quality of life as part of the treatment process. Each treatment plan is tailored to the individual to make the greatest impact on their mental well-being.

IOP for Addiction: How Intensive Outpatient Programs Treat Substance Use Disorders
Charlie Health Editorial Team
Charlie Health data: outcomes among clients with SUD
Clients at Charlie Health are asked to fill out a survey at intake and discharge so that we can monitor their improvements as well as our program quality. This survey includes standardized questions that measure depression symptoms, anxiety symptoms, and suicidal ideation, along with substance use rates. Using this data, we’re able to assess what portion of our population may need help with substance use and the differences in mental health symptoms that they may be experiencing compared to non-substance users.
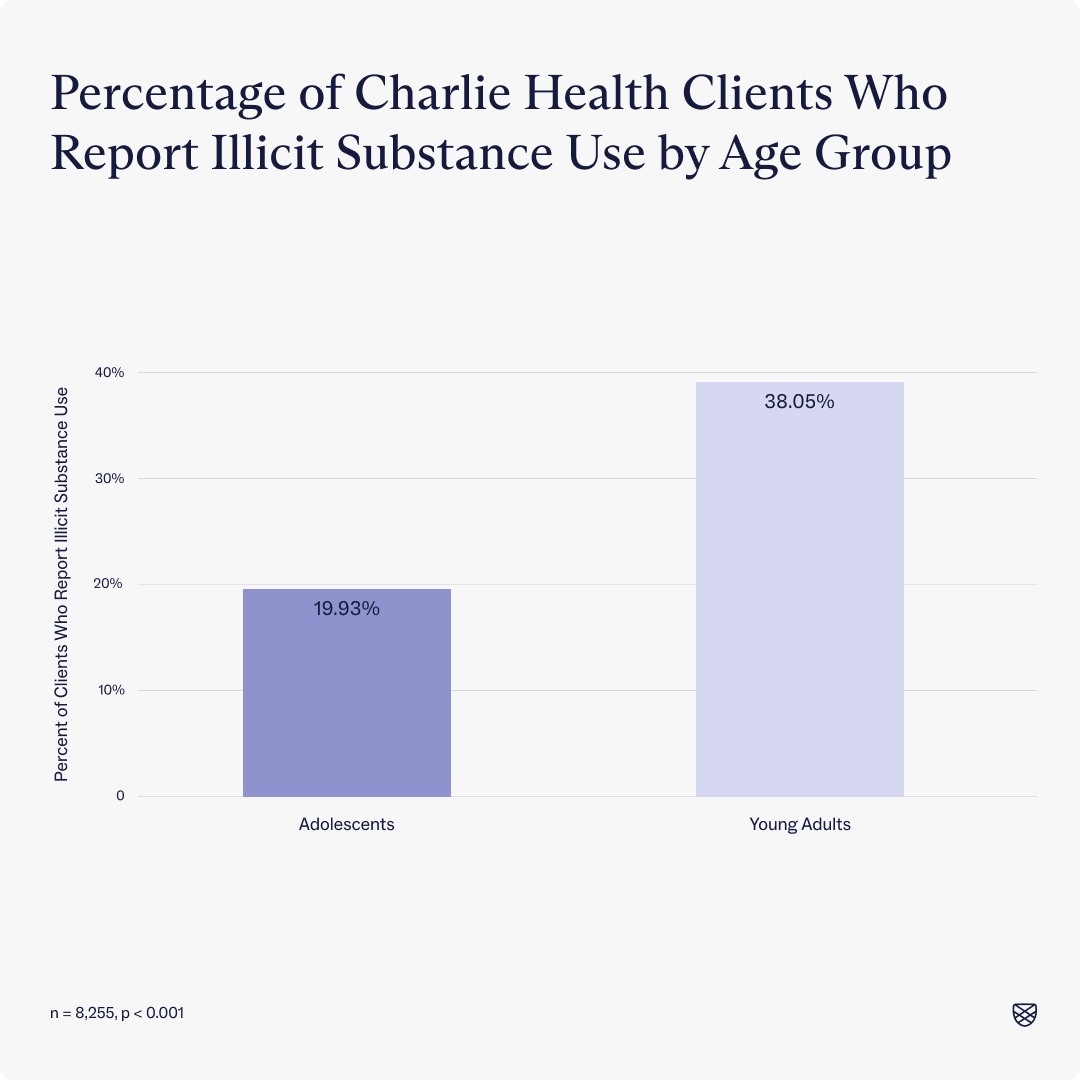
Between January 2024 and June 2024, 29% of Charlie Health clients indicated that they had used non-prescribed or illicit substances in the month prior to intake, with young adult clients (age 18 or over) reporting twice the amount of substance use as adolescent clients.
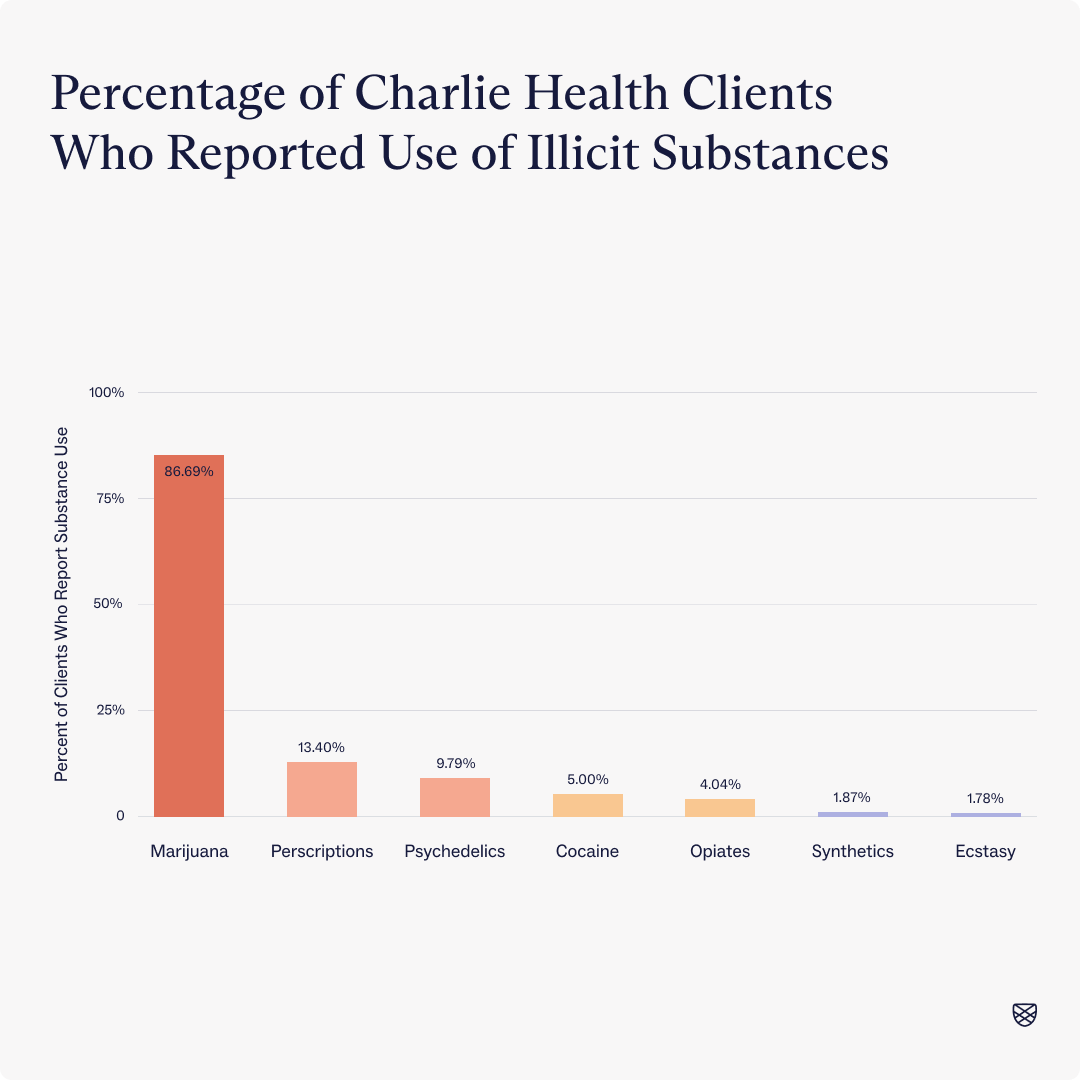
Within that 29% of clients, the most commonly used substance was marijuana.
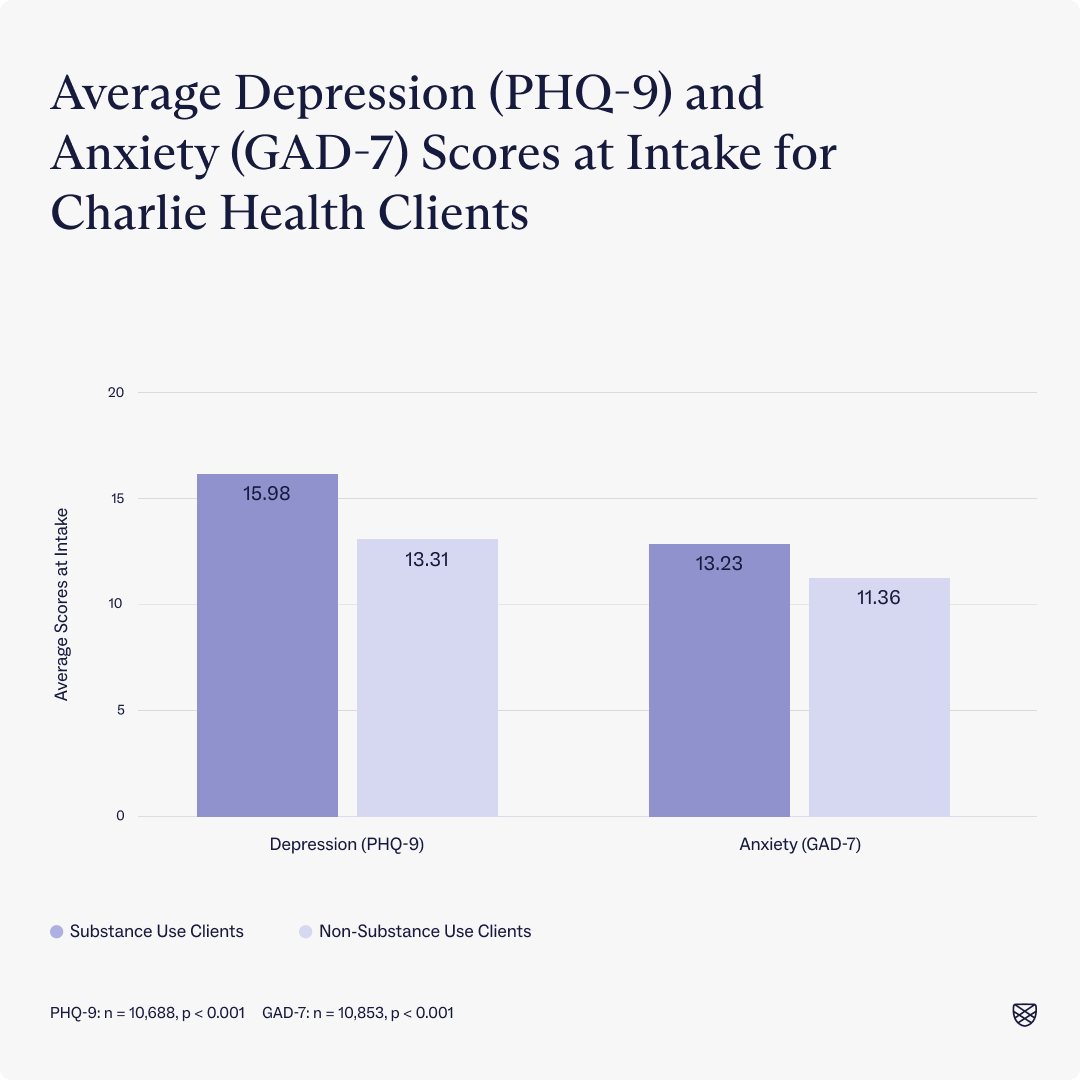
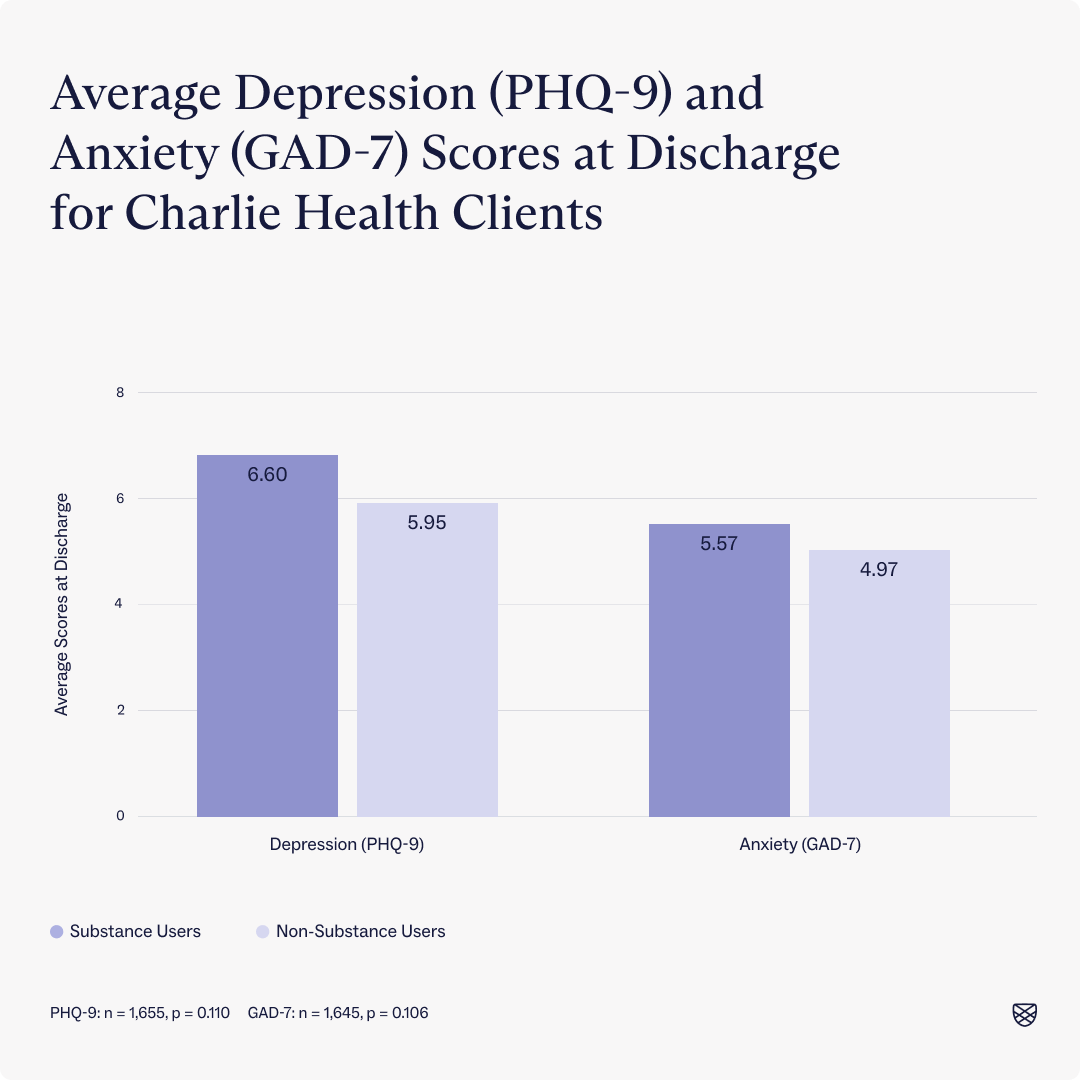
Clients who indicated that they had used substances in the month prior to intake had significantly higher depression scores at intake compared to those who said no to substance use. Similarly, clients who indicated that they had used substances had significantly higher anxiety scores.
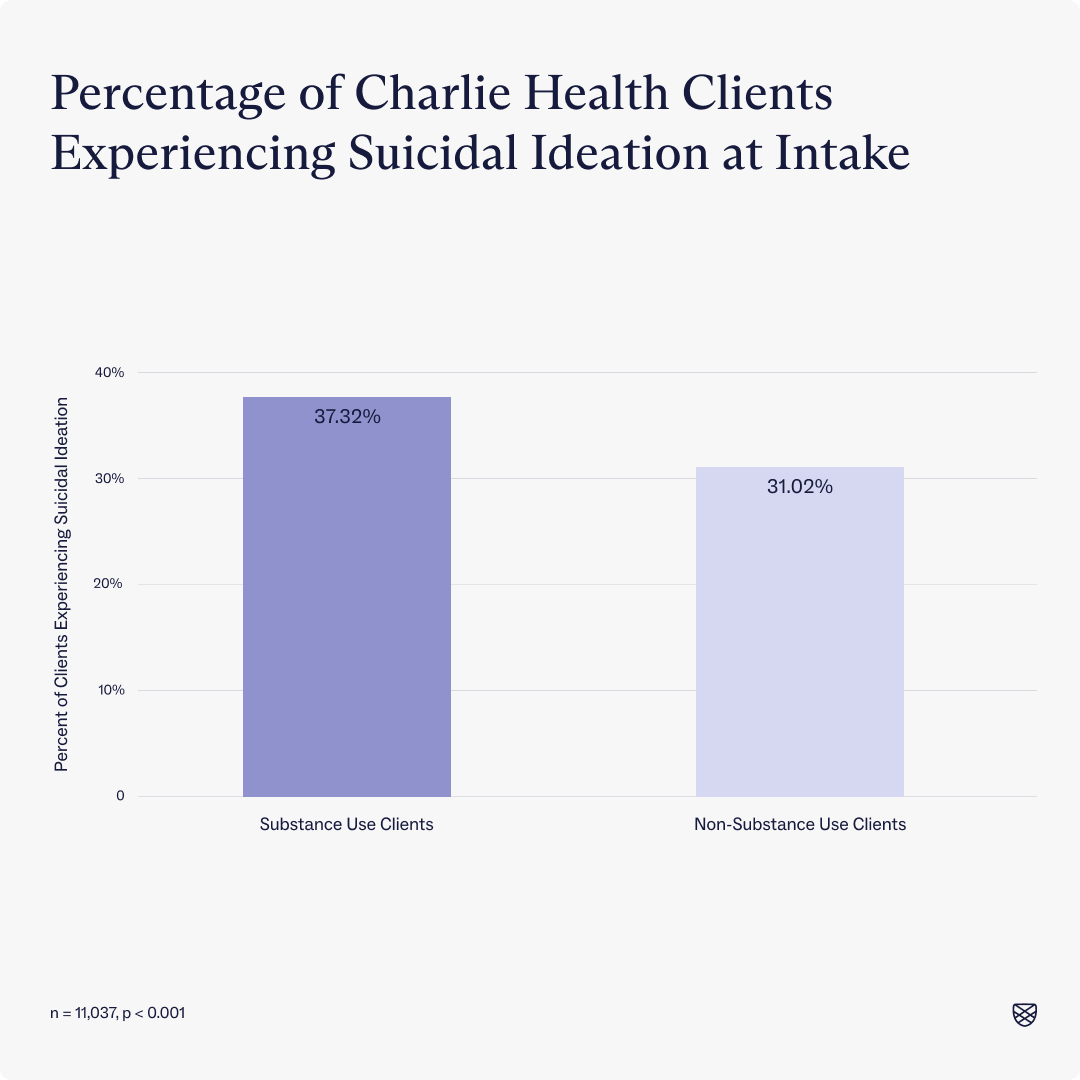
Furthermore, clients who reported substance use also reported higher rates of suicidal ideation than those who did not report substance use.
By discharge, both substance-use clients and non-substance-use clients who completed treatment had average depression scores that fell below the clinical threshold for depression and anxiety.
Furthermore, by discharge, there was no statistically or clinically significant difference in rates of suicidal ideation between our substance-use clients and non-substance-use clients.
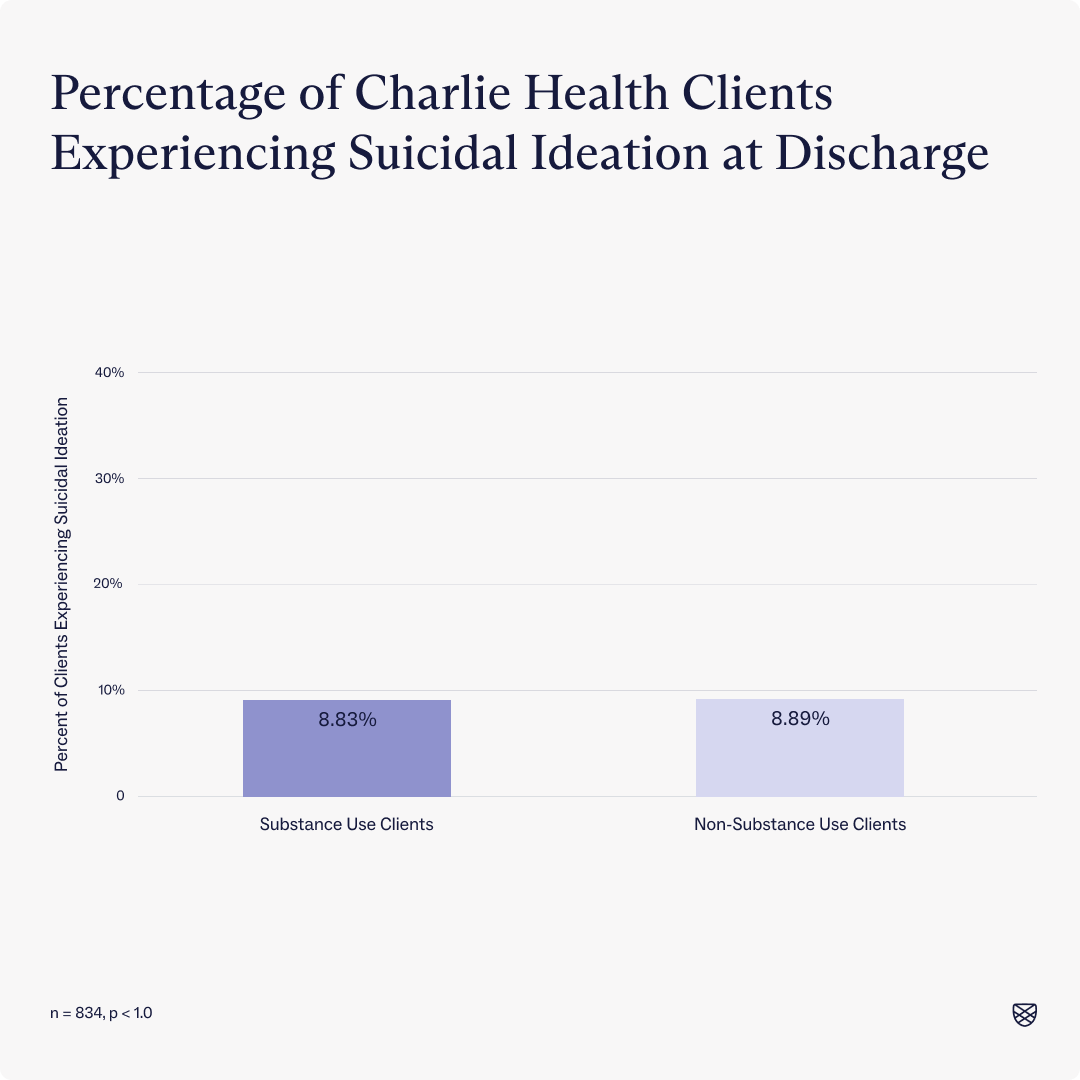
As we see both in the substance use literature and reflected in our own data at Charlie Health, individuals who report substance use in the month prior to intake also report higher acuity symptoms for depression and anxiety, reaffirming the need to treat individuals struggling with substance use holistically. By doing so, our clients see significant improvements both in rates of substance use and depression and anxiety symptoms.

How Charlie Health can help
If you or a loved one is struggling with substance use disorder and co-occurring mental health conditions, Charlie Health is here to help. Charlie Health’s virtual Intensive Outpatient Program (IOP) provides more than once-weekly mental health treatment for young people and families. Our expert clinicians incorporate evidence-based therapies into individual counseling, family therapy, and group sessions. We also offer psychiatric services as needed. With this kind of holistic treatment, managing serious mental health issues is possible. Fill out the form below or give us a call to start healing today.
References
https://www.samhsa.gov/data/sites/default/files/reports/rpt42731/2022-nsduh-nnr.pdf
https://nida.nih.gov/research-topics/trends-statistics/overdose-death-rates
https://www.charliehealth.com/post/what-is-patient-health-questionnaire-9-phq9
https://www.charliehealth.com/post/what-is-generalized-anxiety-disorder-screener-gad7
https://www.charliehealth.com/post/columbia-suicide-severity-rating-scale-cssrs




