
Table of Contents
Is There Gender Bias in Mental Healthcare? Here’s What the Data Shows
Written By: Charlie Health Editorial Team

Clinically Reviewed By: Dr. Don Gasparini
February 28, 2024
4 min.
Data that highlights how gender bias affects mental healthcare, from treatment to access.
Learn more about our Clinical Review Process
Table of Contents
The mental health of those who do not identify as men has long been misunderstood and stigmatized, even leading to disproportionately harsh treatment. In ancient times, “hysteria” (derived from the Greek word for “uterus”) was coined to describe a range of symptoms seen as unusual for women—from heightened emotions to seizures—for which treatment included sex. A stigma associated with this term has persisted well into the modern age. The condition was only removed from the Diagnostic and Statistical Manual of Mental Disorders (DSM) in 1980.
Incredibly, women were largely excluded from scientific healthcare research before 1990 and weren’t required to be included in National Institutes of Health-funded studies with humans until 1993. This long-time research disparity has contributed to ongoing research gaps and care gaps for those who don’t identify as men.
To assess how gender bias impacts mental healthcare, Charlie Health looked at the numbers, including statistics on medication prescription rates across genders and data on cost-related barriers faced by women seeking mental healthcare.
Join the Charlie Health Library
Get mental health updates, research, insights, and resources directly to your inbox.
You can unsubscribe anytime.
It’s important to note that the data included in this piece was collected using a binary understanding of sex and gender, excluding important information about non-binary and transgender people. This exclusion reinforces healthcare disparities for gender-diverse people, deepening the marginalization they already face when seeking care.
The wage gap makes mental healthcare less accessible for those who don’t identify as men
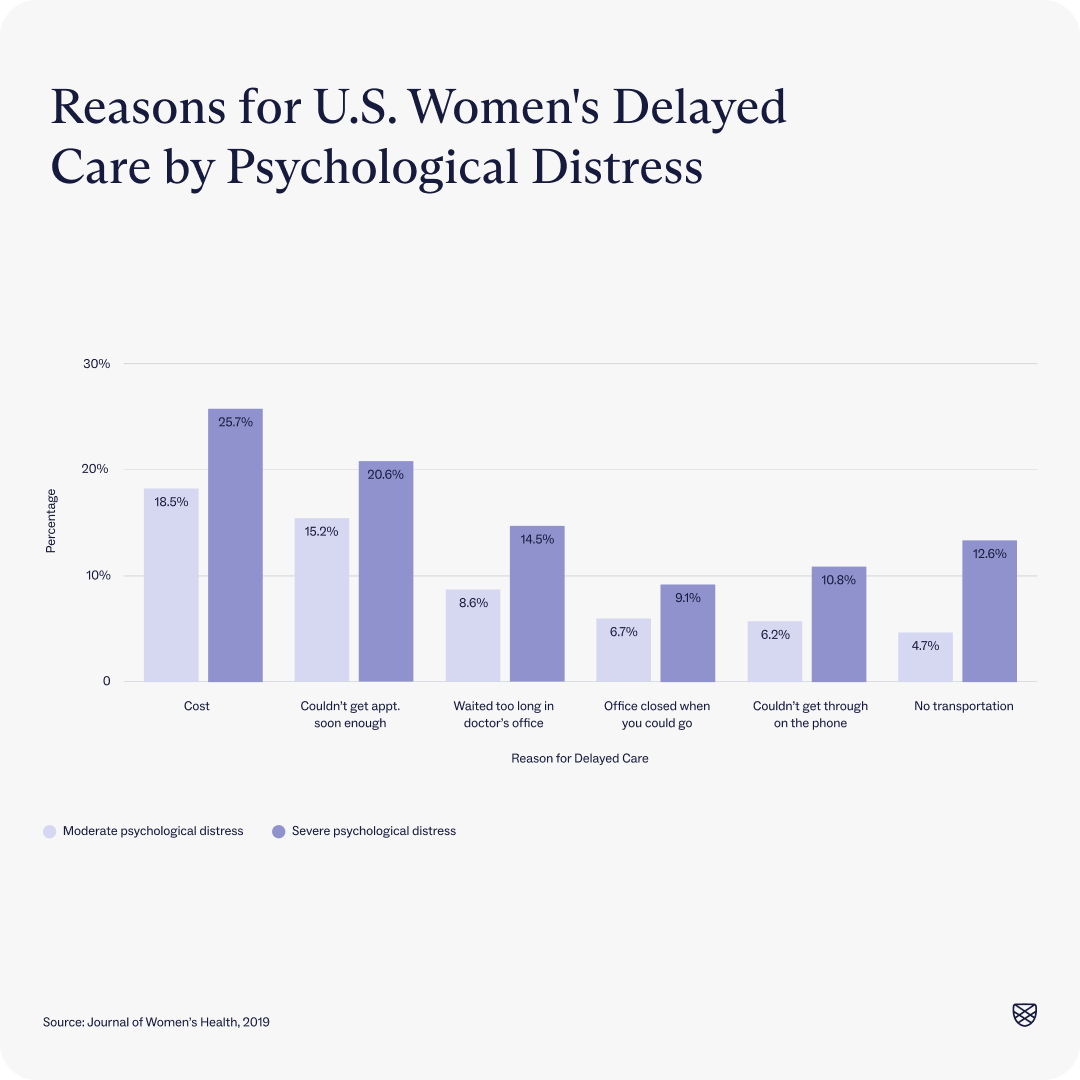
Women earn about one-fifth less than men on average, with larger gaps for women of color, women with disabilities, and gender-diverse people. Income is both a risk factor for mental health issues, according to the American Psychiatric Association, and makes accessing care more challenging. Essentially, those who aren’t men face disproportionate cost-related barriers when it comes to accessing mental healthcare because of the wage gap. One study to this effect found that cost is the greatest barrier to accessing timely mental healthcare for women experiencing moderate psychological distress and severe psychological distress.
The dearth of female mental health providers may impact patient outcomes
While increasing numbers of women are becoming doctors, there are still more male physicians, especially in certain fields. Data shows that this provider imbalance can actually impact patient outcomes. In cardiology, for instance, only about one in 10 providers is a woman, leading to, at times, dire consequences. Female cardiology clients are less likely to get the right treatment when risk factors go unmanaged and are more likely to die from a heart attack if treated by male doctors, studies show.
Gender concordance (when a physician and patient have the same gender) is also missing for clients who aren’t men in parts of the mental healthcare landscape. A 2020 study found that, although half of the U.S. population is female, just over one-third of practicing psychiatrists are female, with much lower rates for people (and women) of color. While there’s not much research specifically on gender concordance and mental healthcare outcomes, studies show that other kinds of concordance between providers and clients do affect mental healthcare results.
Women are more likely to be prescribed medication for mental health conditions than men
Research shows that women and men have similar rates of mental health conditions, but there are differences in the way people of those genders receive treatment. For instance, women are more likely to be prescribed psychotropic medications than men.

Women are also more likely to be diagnosed with depression
Another difference in the treatment provided to women as compared to men comes at the point of diagnosis. Data shows that medical professionals are more likely to diagnose women with depression than men, even when both genders have the same symptoms or similar scores on standardized depression tests.
How to address gender bias in mental healthcare
Addressing gender bias in mental healthcare is, first and foremost, a systemic issue. Above all, providers, researchers, and lawmakers need to raise awareness of how gender bias impacts treatment and advocate for equitable services across the board. Below are some other steps that can be taken to address gender bias in mental healthcare.
Consider sex and gender in research
Many studies don’t account for outcome differences based on sex or gender, but this so-called “neutral” research overlooks important differences that may impact treatment outcomes. For instance, women of childbearing age are regularly left out of drug-related studies and trials (despite many pregnant women using antidepressants during pregnancy), leading to inconsistent and insufficient information on psychotropic medication use during pregnancy. Similarly, mental health research often overlooks gender-specific factors like intimate partner violence. Research funding and academic leadership play a role in this gender-neutral approach, and many experts are calling for a shift towards considering sex and gender in mental health research to improve treatment outcomes.
Improve mental health literacy
Having an understanding of mental health conditions and mental healthcare options can actually improve mental health outcomes. According to one study, increased mental health knowledge is correlated with recognizing the need for mental healthcare and seeking mental healthcare when needed. Although women tend to seek mental healthcare more often than men, mental health literacy remains an important tool for ensuring people of all genders get the care they need.
Seek gender-affirming mental healthcare
It’s important to connect with a mental healthcare provider who is gender-sensitive and committed to meeting your needs. One way to do this is to specifically look for providers or organizations focused on mental healthcare for women or gender-diverse people. If you’re looking for more than once-weekly mental health support from gender-affirming clinicians and others who get it, consider Charlie Heath.
References
https://www.sciencedirect.com/science/article/abs/pii/S0738399113002760
https://pubmed.ncbi.nlm.nih.gov/32705570/
https://www.aamc.org/news/press-releases/majority-us-medical-students-are-women-new-data-show
https://pubmed.ncbi.nlm.nih.gov/31509160/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2828159/
https://www.pnas.org/doi/full/10.1073/pnas.1800097115
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3480686/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4624369/
https://pubmed.ncbi.nlm.nih.gov/20160159/
https://pubmed.ncbi.nlm.nih.gov/23674318/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4802845/
https://www.dol.gov/newsroom/releases/osec/osec20230314
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6743083/
https://www.hrc.org/resources/the-wage-gap-among-lgbtq-workers-in-the-united-states
https://archpublichealth.biomedcentral.com/articles/10.1186/s13690-023-01228-7
https://www.thelancet.com/journals/lanpsy/article/PIIS2215-0366(16)30209-7/fulltext




