
Table of Contents
How Charlie Health Supports Clinician Well-Being

Written By: Elizabeth Kroll

Clinically Reviewed By: Erin Husting
November 25, 2024
5 min.
Learn about how Charlie Health supports clinicians in maintaining well-being and preventing burnout.
Learn more about our Clinical Review Process
Table of Contents
Charlie Health currently employs over 1,300 mental health providers, from Primary Therapists to Crisis Managers to Psychiatrists. While we could not be more honored that these practitioners call Charlie Health home, the mental health workforce as a whole is highly impacted by burnout, leading to low retention rates. Our goal at Charlie Health is to provide comprehensive care and support to our clinicians so they can continue to support our clients, and that starts with understanding burnout and its effect on work. Read on to learn more about how burnout can impact clinical practice and what Charlie Health is doing to improve clinician well-being.

Become a Charlie Health clinician
Competitive benefits, flexible scheduling, and fully remote work.
What is burnout?
Burnout is a state of emotional, physical, and mental exhaustion often caused by prolonged stress or being overworked. According to experts, symptoms of burnout include:
- Feelings of exhaustion
- Feeling cynical about work
- Feelings of hopelessness
- Feelings of resent
- Feelings of uselessness
- Irritability
- Poor sleep
- Trouble concentrating
- Increased headaches
- Taking on more and more responsibilities to try to regain a feeling of fulfillment
A lack of control over your job or career, working in an organization with poor communication skills, having ambiguous job responsibilities, or not receiving enough recognition at work can also lead to burnout. For clinicians specifically, high levels of administrative work have been shown to be associated with burnout as they either increase workload or decrease the amount of time that a clinician can spend with clients, therefore reducing the amount of satisfaction or purpose that they get out of their career.
Who is impacted by burnout in the clinical setting?
According to the research, as much as three-quarters of mental health clinicians (75%) experience burnout during their careers. Many cite feeling overworked, with over half of clinicians (53%) indicating that they worked more in 2022 than in 2021. This trend reflects the growing demand for mental health services, leaving many clinicians stretched thin and struggling to keep up. The emotional toll of consistently managing complex cases can exacerbate feelings of exhaustion and depletion.
Additionally, experts report that clinicians increasingly report feeling as if they don’t have the capacity or skills to meet the current demands of mental health treatment. Without adequate support and resources, these challenges can significantly impact both their professional effectiveness and personal well-being.
However, burnout doesn’t only impact the clinicians themselves. Research has shown that when a clinician experiences burnout, their clients suffer as well. Clients who are treated by a burnt-out clinician are less likely to see improvements in their depression and anxiety scores, data shows. Also, when a clinician becomes so burnt-out that they leave the workforce, their clients are significantly more likely to miss future appointments with their new therapist, according to research. The disruption caused by a clinician’s departure can weaken the therapeutic alliance, a key predictor of treatment success. Clinician burnout can cause mistrust in the therapeutic process, and therefore, the impact of therapy is greatly reduced. Over time, this cycle of burnout and turnover further strains an already overburdened mental healthcare system.

Data: Combating burnout at Charlie Health
At Charlie Health, we always aim to provide our clinicians with as much support as possible to reduce the rates of burnout and improve well-being. Starting this year, we launched a clinician well-being survey that allowed our full-time Primary Therapists to report on their well-being, stress levels, and self-care behaviors in a confidential way so they would feel safe providing accurate information.
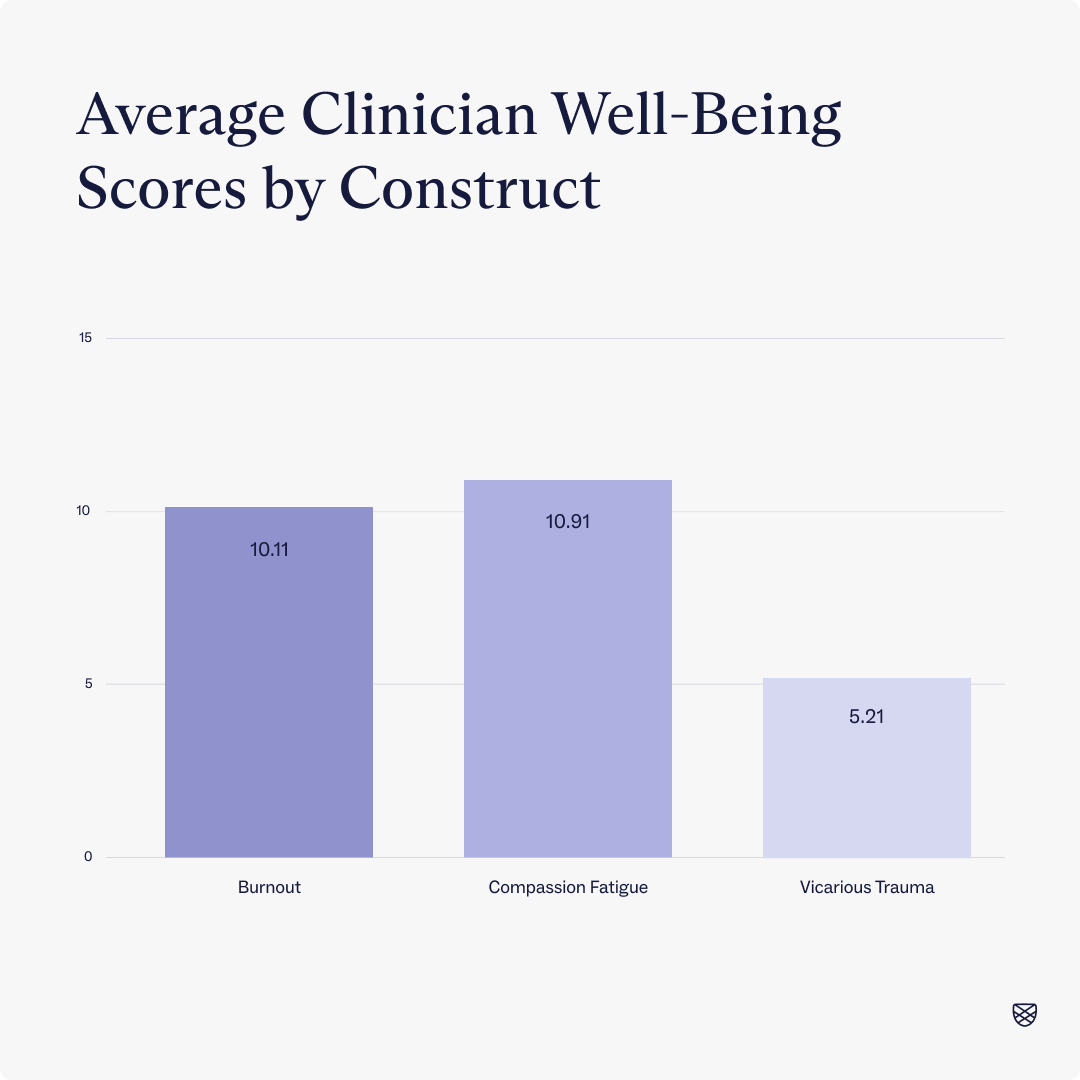
Overall, we found that average rates of burnout, compassion fatigue, and vicarious trauma were low among our full time therapists. On a scale of 0-35, Charlie Health clinicians reported an average score of 10 for burnout and compassion fatigue, and a score of 5 for vicarious trauma. Both of these scores fall into the low-risk category on the scale.
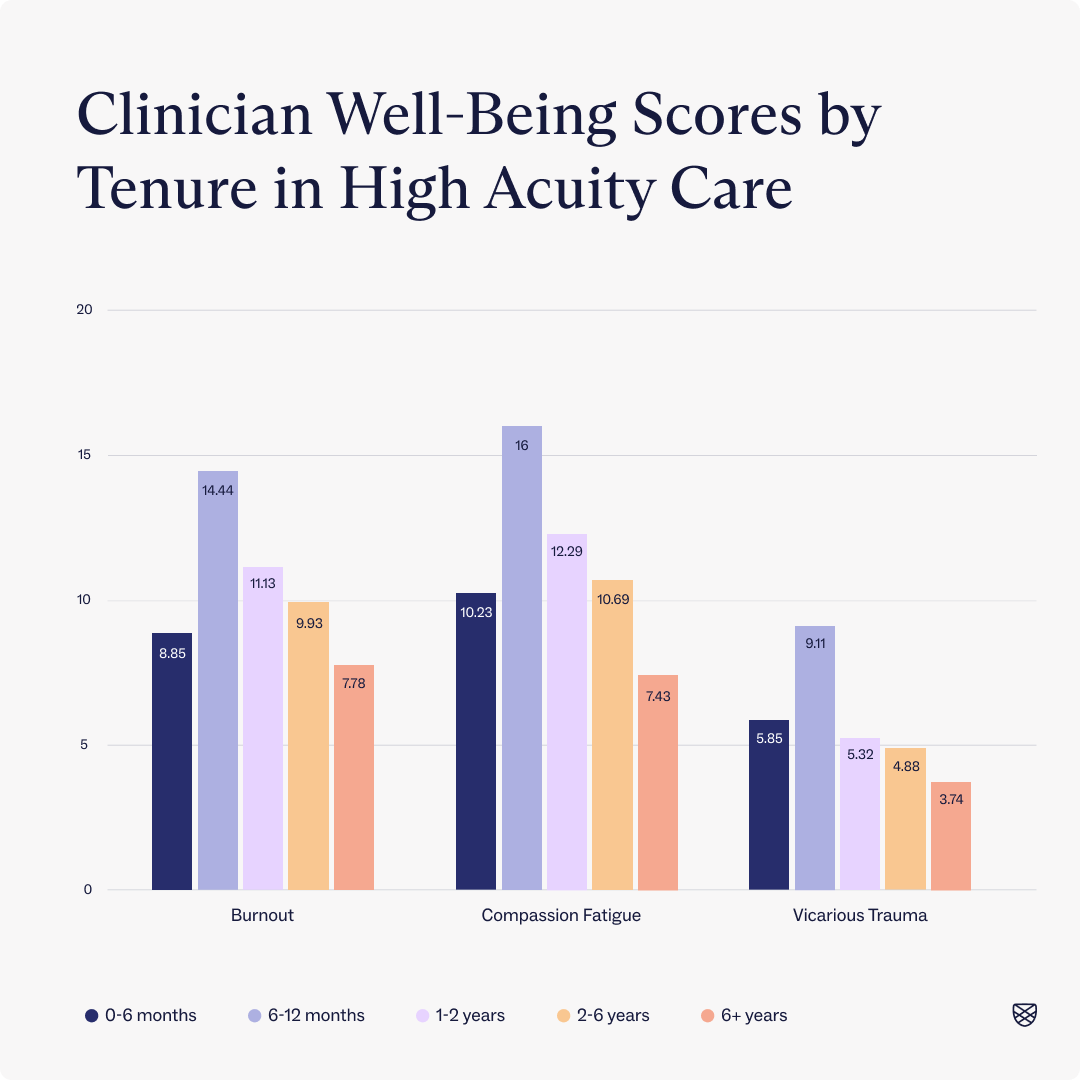
Data also shows that rates of burnout, compassion fatigue, and vicarious trauma are highest for clinicians who have been working in high acuity care for less than a year. Scores for clinicians who have worked in high-acuity care for 6-12 months have burnout and compassion fatigue scores that fall into the moderate risk range, and are approximately 45% higher than the overall average.
But we didn’t stop at well-being scores. We also wanted to know if there were any self-care behaviors or themes that positively impacted clinician well-being so that we could build interventions and scaffolding for our clinicians in the most impactful way.
Results showed that working in a supportive environment and practicing mindful awareness were the two most impactful self-care interventions for well-being, indicating that the more often these self-care behaviors are practiced, the better a clinician’s wellbeing will be.
Maintaining a supportive environment consists of setting good work-life boundaries and building a culture of growth and open communication. As mentioned, data shows that higher levels of supportive structure were strongly linked to lower burnout.
Mindful awareness refers to the practice of intentionally focusing your attention on feelings and emotions with openness and curiosity as opposed to judgment. While mindful awareness also appeared helpful, its impact was less pronounced than that of a supportive environment when stricter statistical methods were applied to confirm the results. However, when done together, these behaviors and skills can significantly reduce rates of burnout, compassion fatigue, and vicarious trauma.
Supportive environment examples
Mindful awareness examples
Maintaining a manageable schedule
Maintaining a balance between what others expect and what you feel is important
Maintaining an organized environment
Encourage Open Communication
Taking part in professional development
Maintaining a manageable schedule
Maintaining a balance between what others expect and what you feel is important
Maintaining an organized environment
Encourage Open Communication
Taking part in professional development
As explained, the increasing burnout of mental health clinicians is leading to an even more strained healthcare system, which threatens to impact clients. While full-time Primary Therapists at Charlie Health indicate a low risk of burnout, compassion fatigue, and vicarious trauma, we are still constantly working to improve their working conditions to ensure longevity in their careers so that they can help as many patients as possible throughout their lifetime.

Join Charlie Health’s Clinical Team
If you’re passionate about making an impact on the national mental health crisis and are motivated by a desire to learn and grow, apply to join the Charlie Health team today. We have nationwide openings for clinicians across the spectrum of licensure and offer flexible scheduling, fully remote work, and other competitive benefits. Together, we can provide the world with life-saving mental healthcare.
References
https://www.umassmed.edu/globalassets/office-of-community–government-relations/dynamic-futures/documents/mental-health-weekly—dynamic-futures.pdf
https://www.apa.org/pubs/reports/practitioner/2022-covid-psychologist-workload.pdf
https://onlinelibrary.wiley.com/doi/full/10.1002/da.22766
https://www.sciencedirect.com/science/article/abs/pii/S0190740918301683
https://www.mayoclinic.org/healthy-lifestyle/adult-health/in-depth/burnout/art-20046642



