
Table of Contents
How Charlie Health’s Virtual IOP Improves Clients’ Physical and Mental Health

Written By: Komal Kumar, MS

Clinically Reviewed By: Dr. Don Gasparini
October 5, 2023
7 min.
Charlie Health's holistic model of care leads to substantial improvements in both mental and physical well-being with the use of personalized treatment. Read more about clients’ outcomes and the mind-body approach taken at Charlie Health.
Learn more about our Clinical Review Process
Table of Contents
The relationship between mental health and physical health
Mental health and physical health are inextricably linked. Although the relationship is not fully understood in the medical world, having poor mental health can increase one’s chances of developing chronic physical symptoms, and having poor physical health can increase one’s chances of developing serious mental health conditions.
Historically, mental and physical health were regarded as separate entities within Western medical systems, with much more focus placed on treating physical health conditions. This is slowly changing, though, as an influx of emerging research in the field supports the link between mental and physical health.
For example, a study examining the association of mental and physical health problems in high-risk adolescents found that young people with mood and behavior disorders were more likely to have infectious diseases, respiratory problems, and weight problems. In another study on the link between mental health and heart health, those with mood and anxiety disorders showed significantly reduced heart-rate variability (HRV), a marker of physical health that can lead to immune dysfunction and inflammation, cardiovascular disease, and mortality long-term. Tens of studies like these now exist.
Research shows that in adolescents experiencing mental health conditions, some of the main bodily symptoms include sleep, memory, focus, stomach aches, headaches, appetite and eating patterns, and physical energy. Charlie Health’s virtual Intensive Outpatient Program (IOP), which serves young people with complex mental health conditions, considers a client’s mental and physical health together in their treatment planning. This holistic, mind-body approach to care is believed to contribute to clients’ positive outcomes during IOP.
Holistic therapy for mind-body healing at Charlie Health
Western healthcare settings are increasingly adopting holistic approaches to mental and physical healing—practices grounded in ancient healing practices, like Traditional Chinese Medicine and Ayurvedic medicine, that have long emphasized the mind-body connection. Examples include biofeedback, meditation, and cognitive behavioral therapy (CBT) to help manage blood pressure and chronic illness symptoms.
Holistic healing is a cornerstone of treatment at Charlie Health, too. As mentioned, our IOP factors a client’s mental and physical health into creating their treatment plan, and we track clients’ physical and mental health symptoms as measures of success. Also, Charlie Health’s curriculum covers several movement-based therapy modalities. Examples include yoga and dance therapy, both designed to stimulate the mind and body. Other curricula focus on breathwork, progressive muscle relaxation, and somatic reprocessing to help clients address memories stored in the body and soothe the nervous system. At Charlie Health, we understand that nurturing healing through the dual lenses of mental and physical well-being is imperative, for they are fundamentally intertwined—as indicated by our outcomes.

Industry-leading care. Life-saving outcomes.
Robust clinical research results in more personalized care.
Charlie Health data: physical health outcomes for clients
As part of an ongoing quality improvement study at Charlie Health, we collect data from clients using self-reported surveys to follow trends and improve our quality of care. Before starting treatment, Charlie Health clients reported a number of physical health symptoms at intake.
In a sample of 3,643 young people admitted to Charlie Health’s virtual IOP program between June 2021 and August 2023, clients reported trouble with sleep, energy, and tiredness half the days a week or more on average. Clients also reported struggling with focus and concentration, fidgeting or moving slowly, and appetite changes several days a week on average. See a full table of the symptoms and clinical interpretations below:
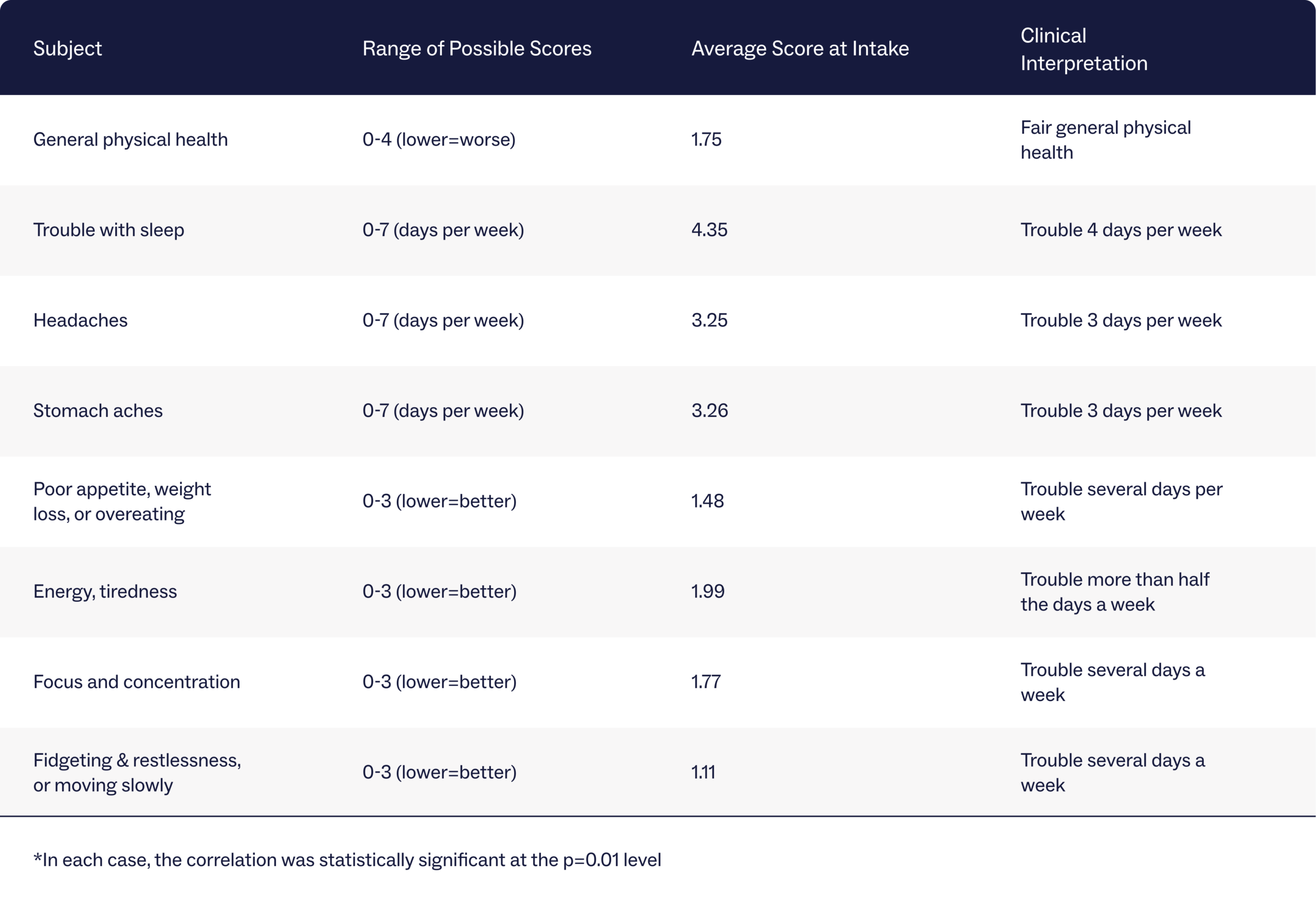
By the end of programming, clients experienced, on average, statistically significant improvements in all of the physical health symptoms listed. Here’s an overview of some of the findings:
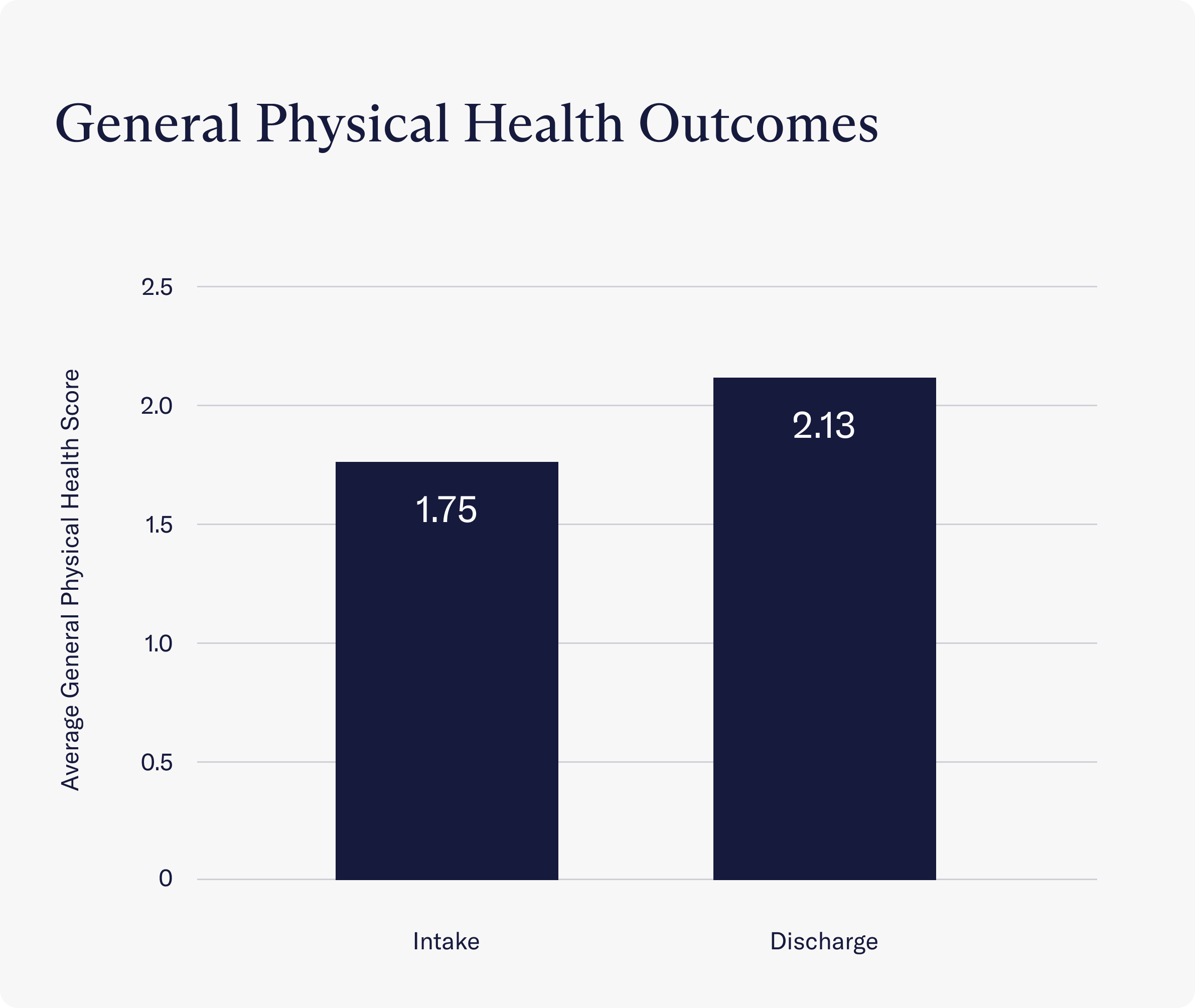
- Clients reported a significant improvement in their general physical health as a result of programming. At intake, clients reported fair physical health (a score of 1.75 on average). After completing IOP, though, clients reported good physical health (a score of 2.13 on average).
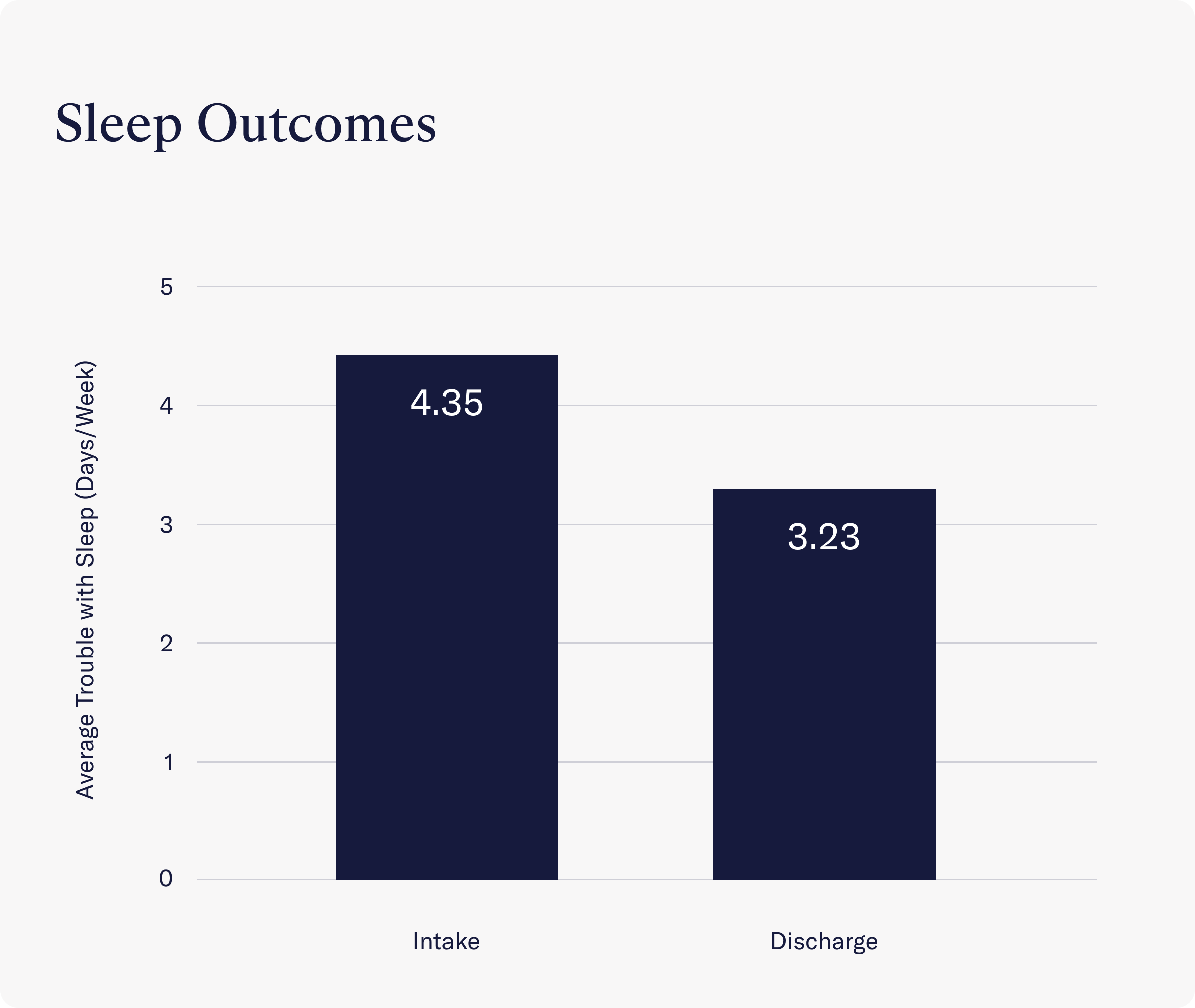
- Clients reported a significant improvement in their sleep problems throughout treatment. Instead of struggling with sleep 4.35 days per week, clients reported sleep struggles 3.23 days per week on average.
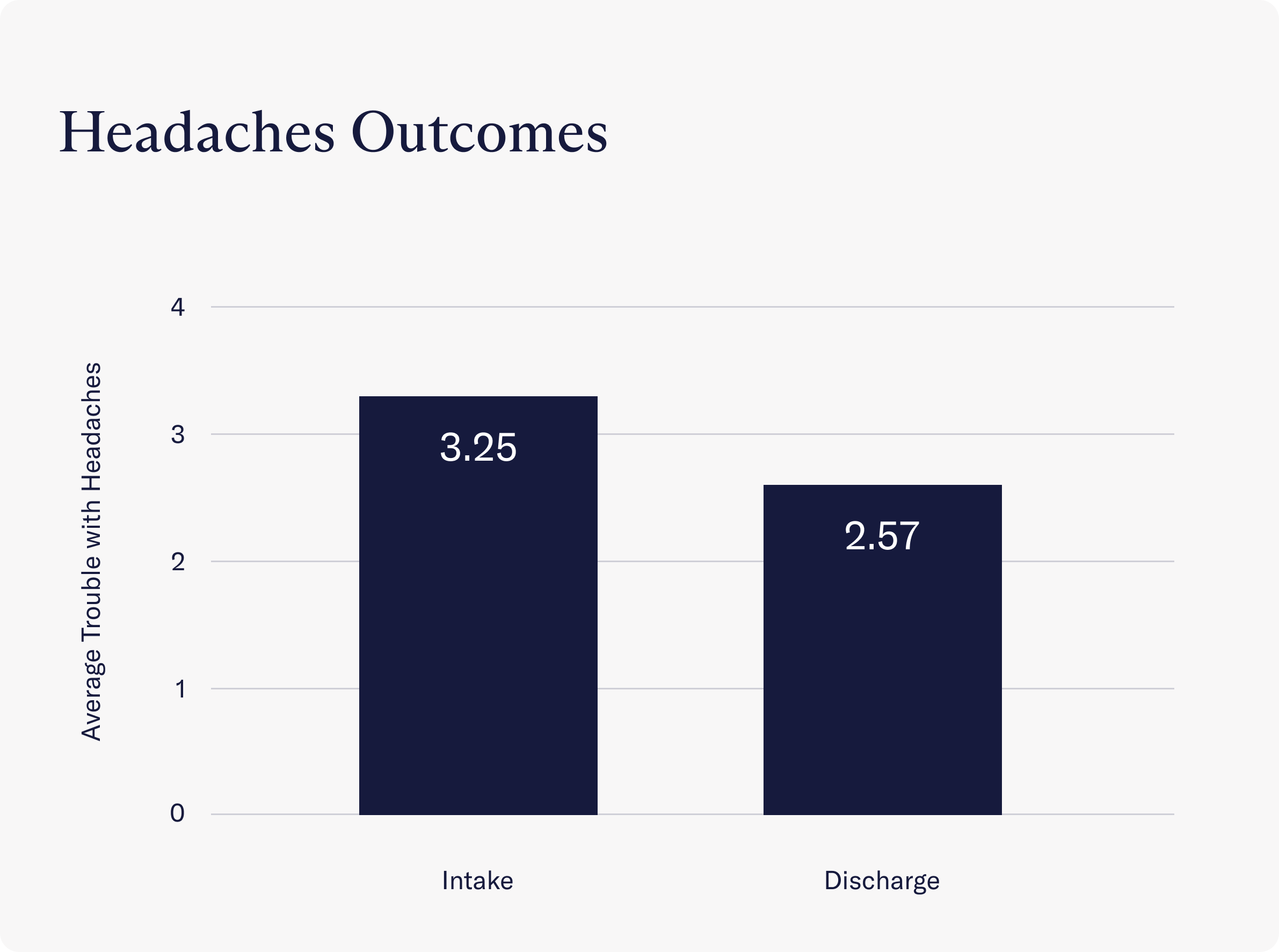
- A significant reduction was seen in the occurrence of headaches. At intake, clients reported experiencing headaches an average of 3.25 days per week, while at discharge, this number fell to 2.57 days per week.
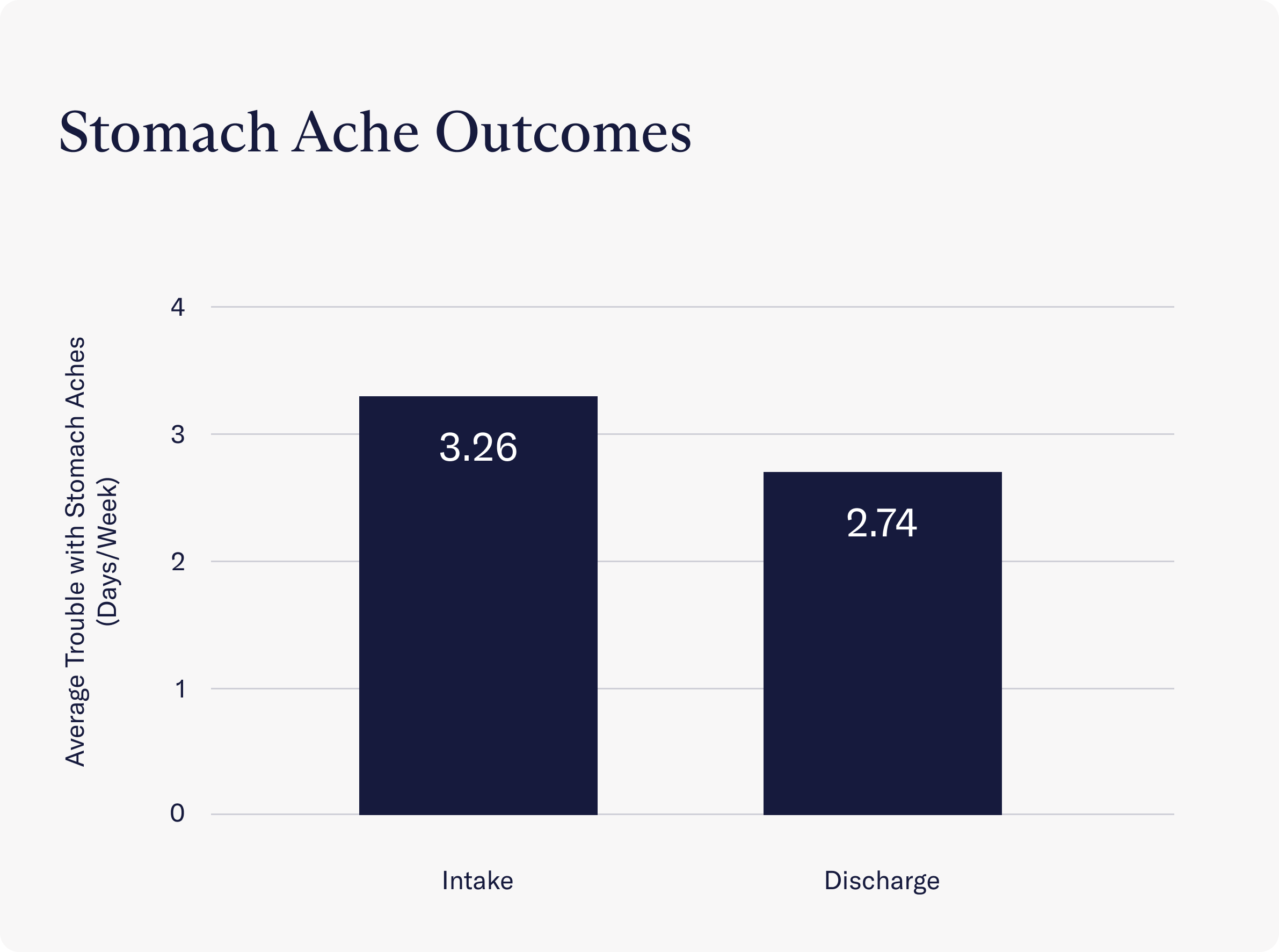
- A significant reduction was seen in the occurrence of stomach aches. At intake, clients reported experiencing stomach aches an average of 3.26 days per week, while at discharge, this number fell to 2.74 days per week.
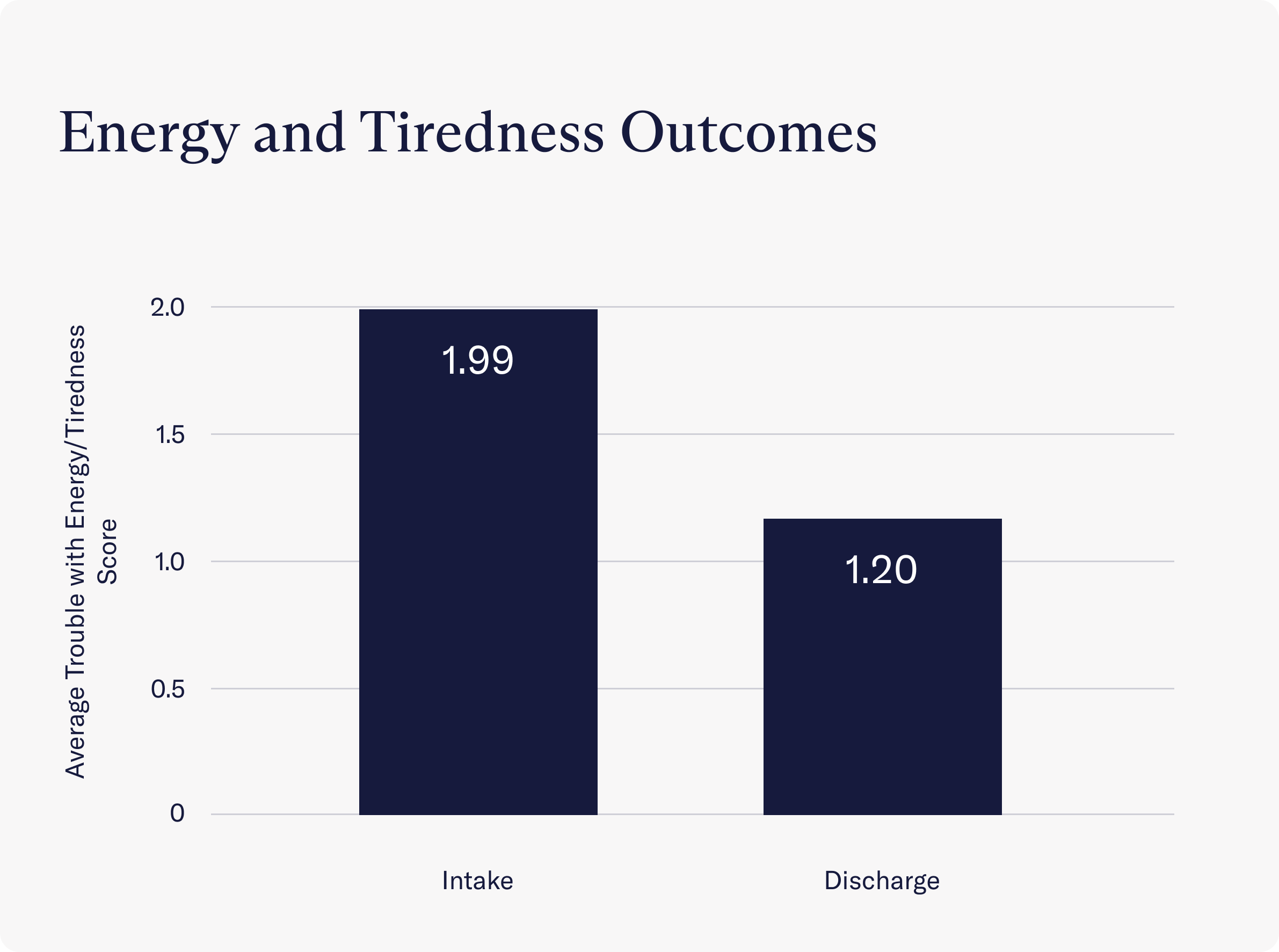
- Clients reported having significantly more energy and feeling less tired due to Charlie Health programming. Instead of struggling with energy and tiredness more than half the days a week (a score of 1.99), clients reported struggling with these symptoms only several days a week (a score of 1.20 on average) by discharge.
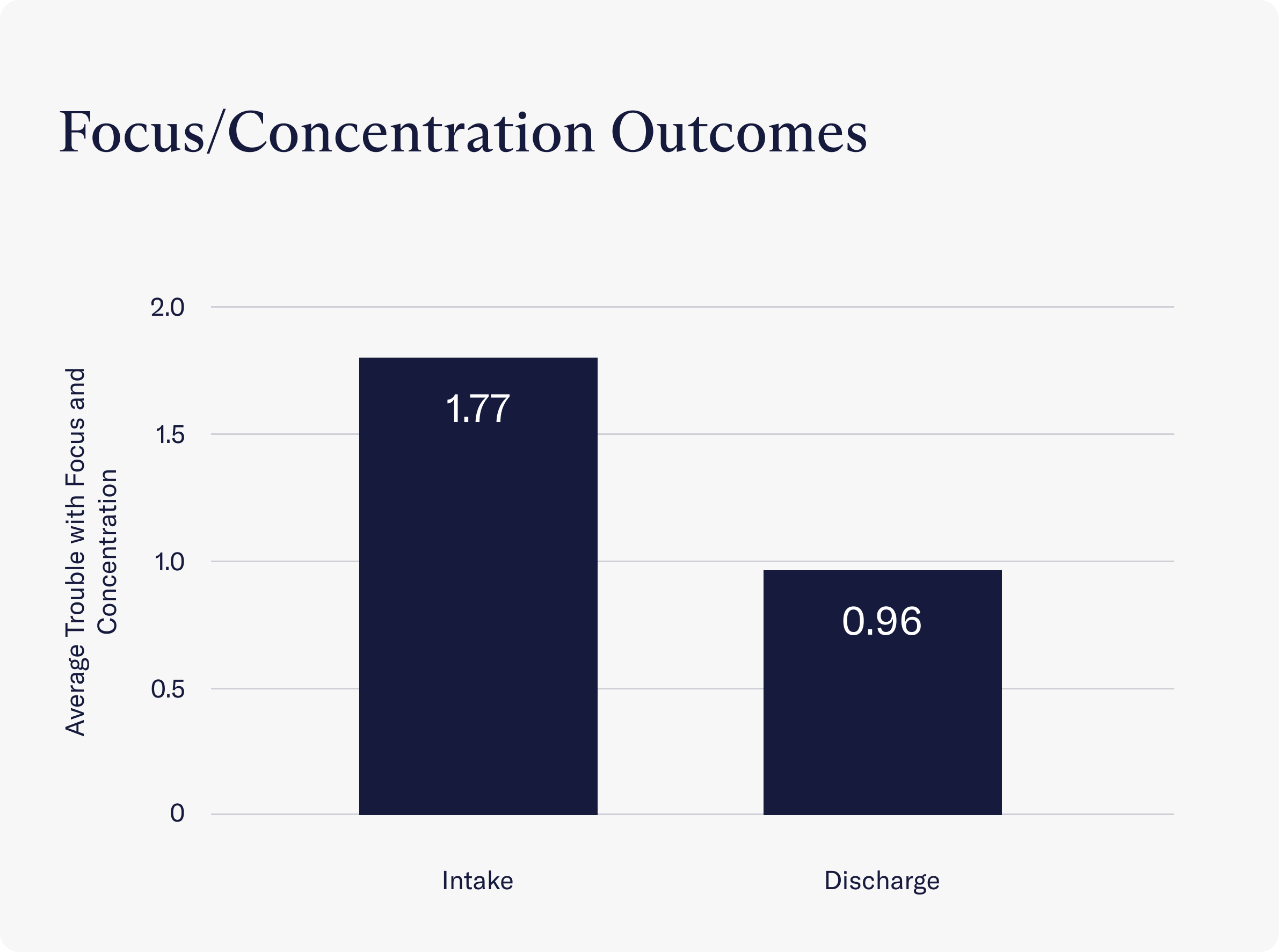
- After completing treatment at Charlie Health, clients reported no trouble at all with focus and concentration on daily activities (a score of 0.96 on average). This was a significant decrease from the score at intake, which showed that clients struggled to focus on daily activities several days a week (a score of 1.77).
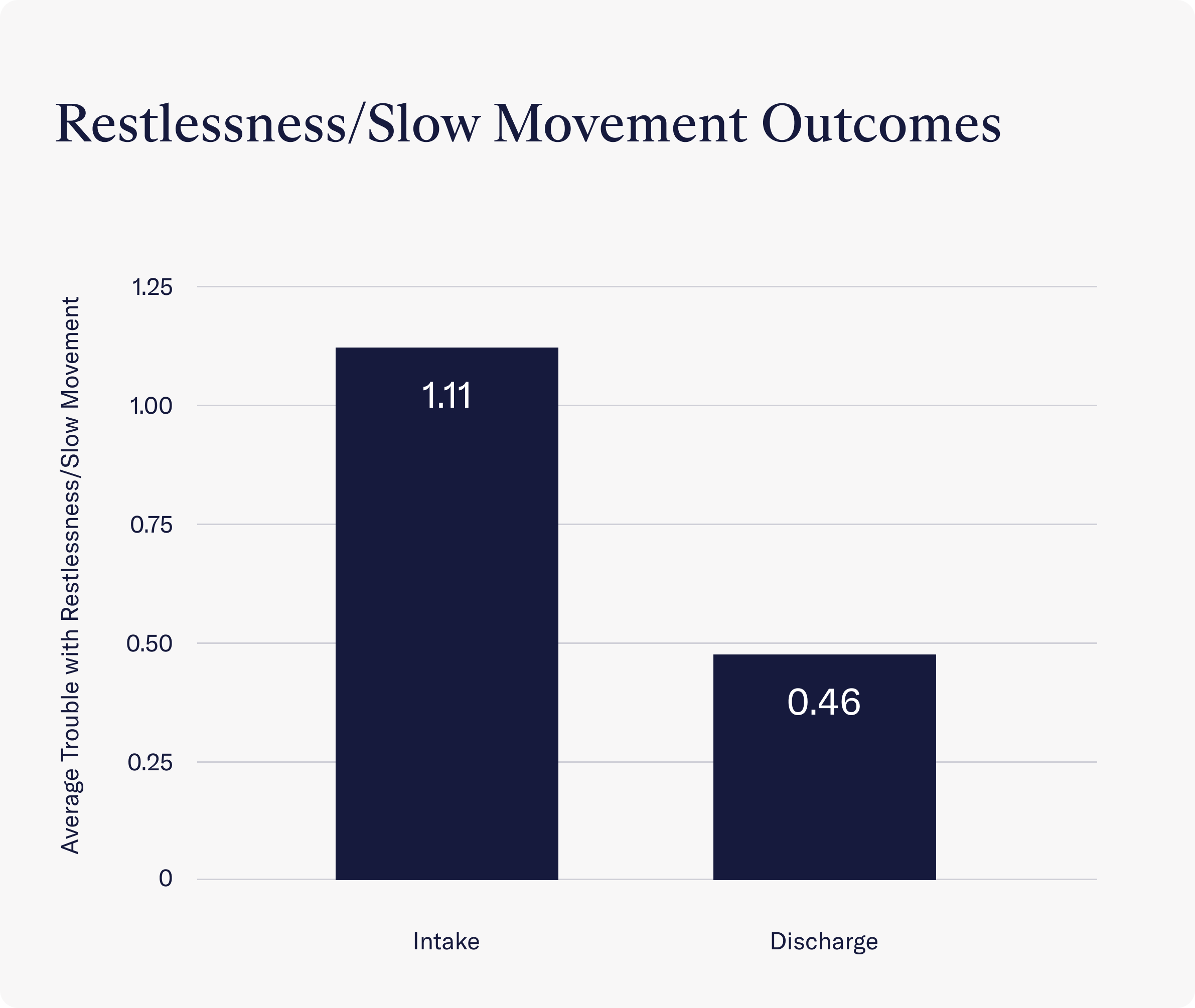
- After treatment, Charlie Health clients experienced significant improvement in terms of feeling either fidgety or restless or moving or speaking too slowly. At intake, clients reported struggling with these symptoms several days a week (a score of 1.11 on average), but by discharge, clients reported no trouble at all in these areas (a score of 0.46 on average).
Charlie Health data: mental health outcomes for clients
Looking more closely at the relationship between mental health and physical health outcomes in the same sample of clients, reductions in mental health symptoms were significantly correlated with reductions in physical health symptoms. That is, the more a client’s mental health improved throughout the course of treatment, the more their physical health symptoms improved as well.
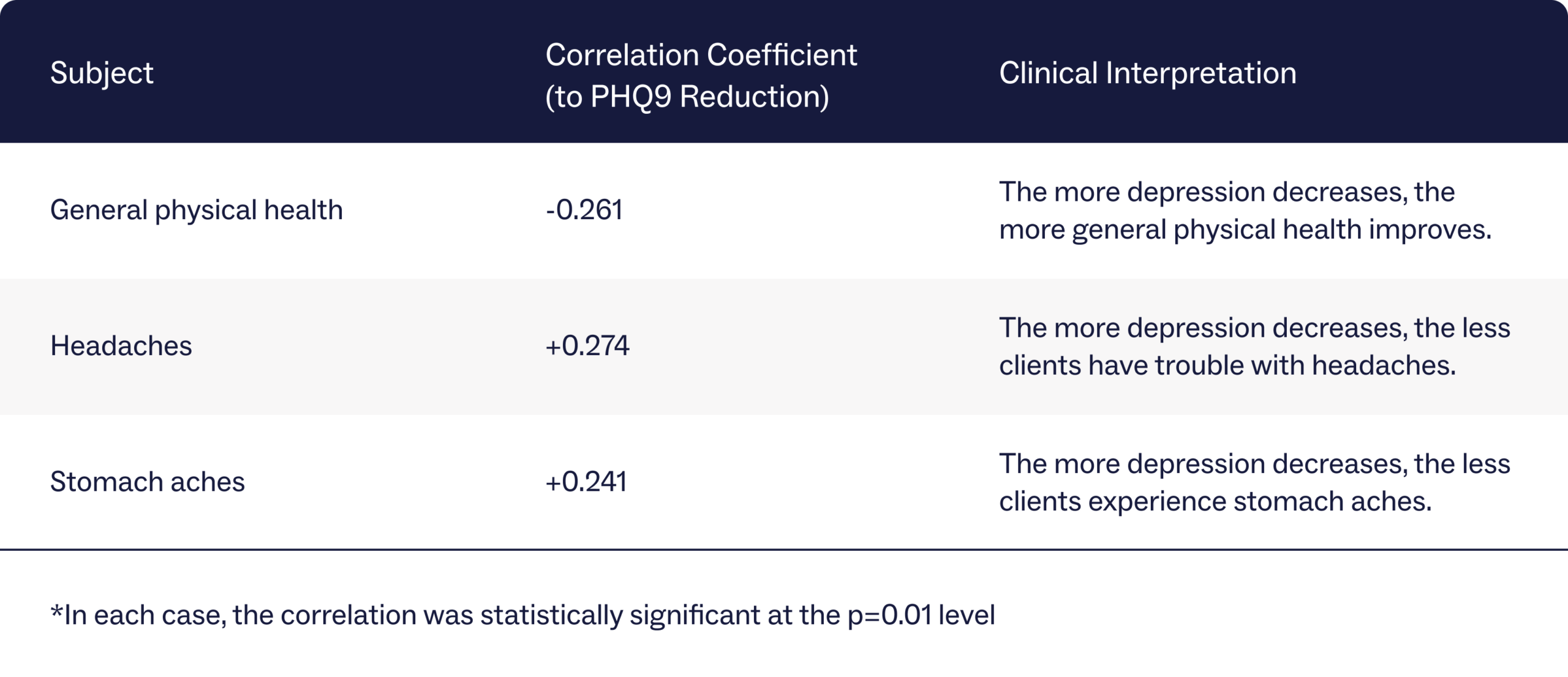
Mind-body outcomes for clients with depression
After receiving holistic care at Charlie Health, clients with depression reported a simultaneous reduction in symptoms of depression and an improvement in physical health symptoms.
Rates of depressive symptoms among clients were measured using the Patient Health Questionnaire-9 scale for depression (PHQ-9), which categorizes depression into five groups ranging from “no depression” to “severe depression.” An analysis of clients’ PHQ-9 scores at intake and discharge compared to health symptoms showed that the more a client’s depression decreased, the more their health improved. Specifically, data shows that a decrease in depressive symptoms correlated with an improvement in general physical health and fewer headaches and stomachaches.
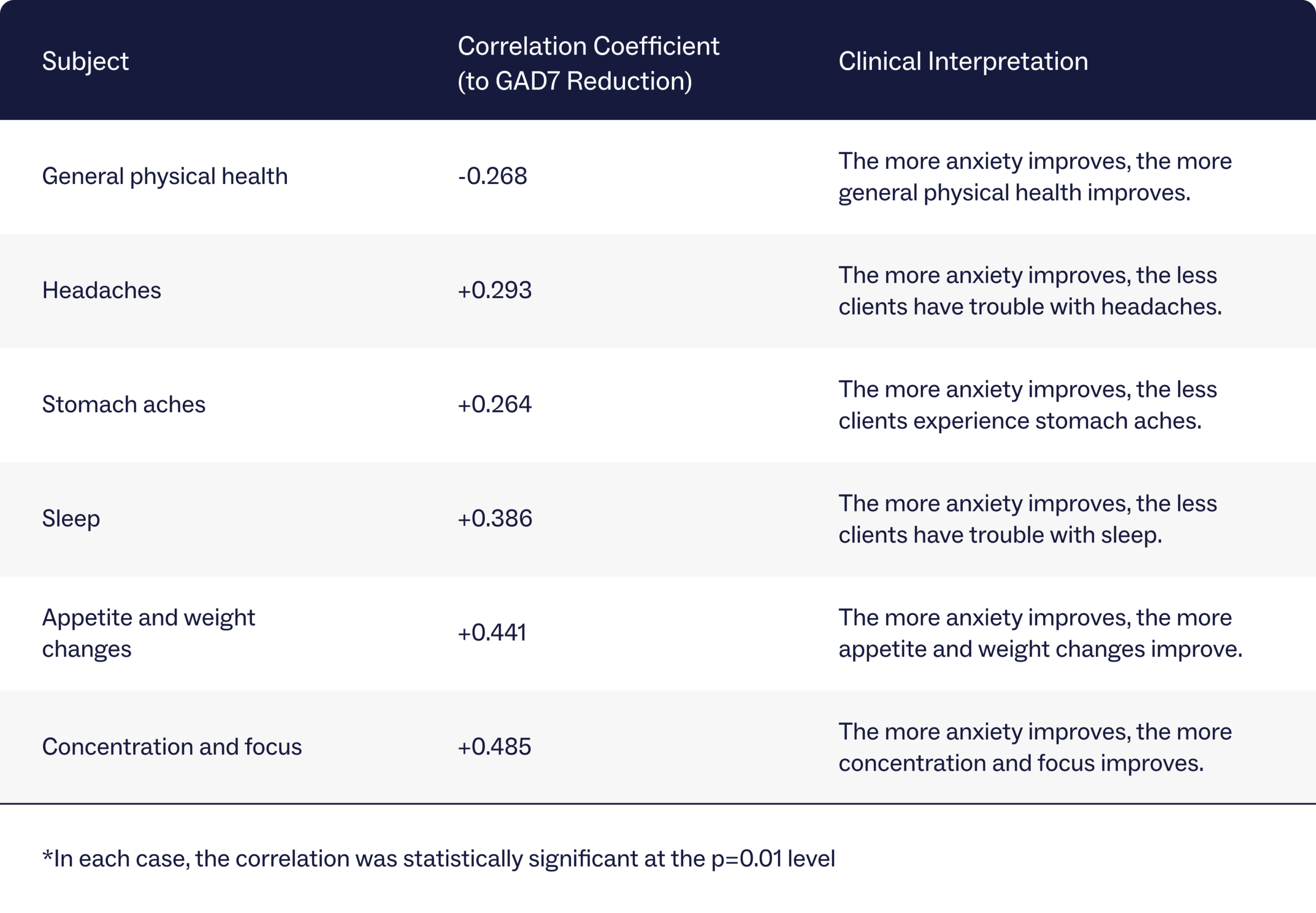
Mind-body outcomes for clients with anxiety
Similarly, clients with anxiety reported improvements in their anxiety and physical health symptoms after treatment at Charlie Health.
Anxiety levels among clients were evaluated using the General Anxiety Disorder-7 (GAD-7), which classifies people into four groups based on anxiety severity, from “minimal anxiety” to “severe anxiety.” Examining clients’ GAD-7 scores at the beginning and end of their treatment compared to health symptoms revealed a strong connection between reduced anxiety and improved overall health. The more a client’s anxiety improved, the more they noted improvements in physical health, relief from headaches and stomach aches, better sleep, stable appetite and weight, and better concentration and focus.
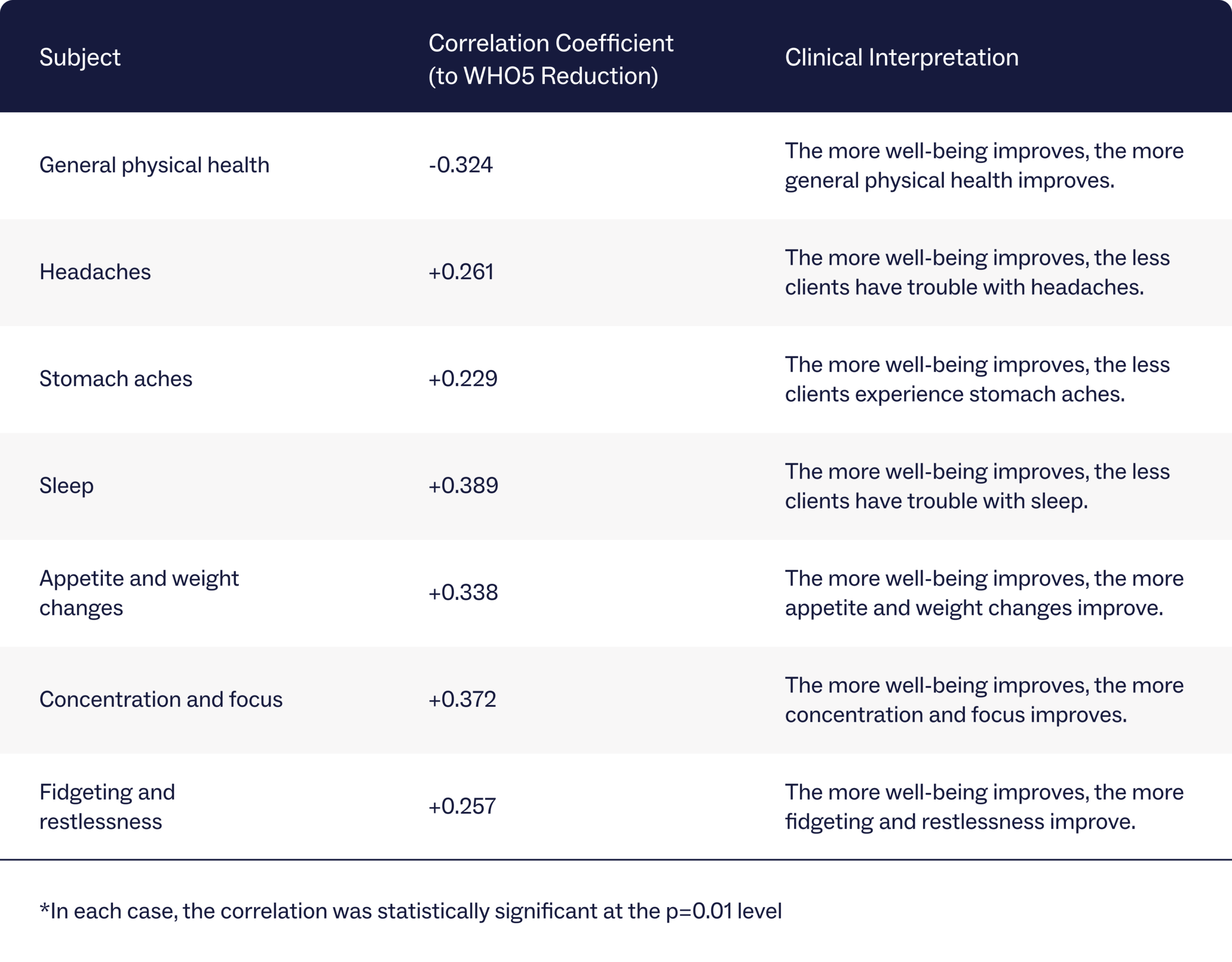
Overall mind-body outcomes for clients
Finally, data shows that the more clients’ psychological well-being improved, the more many bodily symptoms improved.
Clients at Charlie Health used the World Health Organization Five Well-Being Index (WHO-5) to measure overall mental health improvement. This self-assessment measures a person’s well-being by asking questions about their mood over the past two weeks. An analysis of clients’ WHO-5 scores from intake to discharge compared to health symptoms shows a correlation between mental health improvement and physical health improvement.
The more a client’s well-being improved, the more they noted improvements in all observed categories of general physical health, including headaches, stomach aches, sleep, appetite, concentration and focus, and fidgeting and restlessness.
Improving physical and mental health symptoms with Charlie Health’s IOP
As mentioned, Charlie Health holistically approaches patient care, treating both the mind and the body as inseparable to well-being. When one improves, the other improves, and vice versa. The curriculum at Charlie Health aims to treat the entire person, using mental and physical techniques that work hand in hand to produce the best client outcomes.
While causation is generally impossible to determine (Did the mental health condition cause the physical health condition? Or did the physical condition cause the mental health condition?), examining the two together is crucial to providing the most effective care possible. Without knowledge of one or the other, important keys to a client’s treatment plan may be missed.
Charlie Health’s clients struggle with many somatic symptoms at intake, such as trouble with sleep, frequent headaches and stomach aches, dysregulated appetite and weight loss, trouble with concentration, and more. By the end of programming, though, all of these symptoms significantly improve in correlation with mental health symptoms. The more depression, anxiety, and psychological well-being improve, the more somatic symptoms improve as well. These outcomes highlight the undeniable relationship between the mind and the body.
Mind-body support at Charlie Health
If you or a loved one are struggling with complex mental health symptoms that are also affecting your body, Charlie Health is here to help.
Our virtual intensive outpatient program (IOP) combines group sessions, individual therapy, and family therapy, offering more support than once-weekly therapy but less oversight than inpatient treatment. Different therapy modalities—ranging from yoga and meditation to CBT and DBT skills—are used multiple times a week in individual and group settings to provide symptom relief and promote holistic recovery.
Fill out this short form to get started today.
References
https://pubmed.ncbi.nlm.nih.gov/29132081/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6606411/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2768339/
https://www.sciencedirect.com/science/article/abs/pii/S016787601300189X
https://link.springer.com/article/10.1007/s12144-022-03053-7




