
Table of Contents
The Associations Between Marijuana Use and Teen Depression: What You Need to Know

Written By: Colin Crouse

Clinically Reviewed By: Dr. Don Gasparini
July 29, 2023
7 min.
With marijuana more accessible to children and teens in the United States, understanding its potential long-term impact on their mental health is crucial. In this piece we use data to explore how heavy marijuana use relates to heightened teen depression.
Learn more about our Clinical Review Process
Table of Contents
As many states legalize marijuana nationally, with more to follow, weed has become increasingly accessible to children and adolescents. While research shows that occasional weed use is virtually harmless for most developed adults, marijuana use among adolescents and children might have serious long-term repercussions, potentially leading to developmental issues and mental health problems later in life.
Marijuana use in the United States
Marijuana, known more formally as cannabis, is the third most commonly used drug in the United States and is immensely popular among adolescents and young adults. In fact, marijuana use is the highest among young adults and adolescents compared to the rest of the U.S. population. Additionally, people within this age range are at the highest risk of developing mental health conditions like depression, anxiety, and substance use disorder. While weed has been found to have medical benefits, using weed at a young age while the brain is still developing could lead to mental health issues later in life.
Marijuana use among depressed youth
Current academic literature examining the subject of marijuana and its impact on depression is rather polarized. Some studies suggest marijuana, used in specific dosages, could be a potential treatment for depression, while others disagree, arguing weed can exacerbate the symptoms of or possibly cause depression. While the full scope of marijuana’s benefits and drawbacks is still unknown, most researchers can agree that excessive weed use is not good for children and adolescents. Studies have shown heavy marijuana use, defined as multiple times per week, among adolescents is associated with higher rates of depressive symptoms and suicide attempts.
Join the Charlie Health Library
Get mental health updates, research, insights, and resources directly to your inbox.
You can unsubscribe anytime.
The age at which someone starts using marijuana is also a strong determining factor for mental health outcomes later in life. The younger someone is when they start using weed, the more at risk they are of developing a future mental health condition. In fact, a study conducted at Columbia University found teens who use marijuana recreationally are two to four times more likely to develop a psychiatric disorder such as depression later in life. Furthermore, other studies examining the cognitive impacts of marijuana use in adolescents have found that prolonged weed use can lead to reductions in cognitive functioning.
No concrete data supports the theory that marijuana directly causes depression, but recent studies have found heavy marijuana use may exacerbate the symptoms of depression. A study conducted in 2021, for instance, found that marijuana use among individuals with depression was associated with an increase in depressive symptoms. A similar study also concluded that marijuana use worsened depressive symptoms and was associated with overall poorer mental health in individuals already struggling with mental health issues.
While an association between marijuana and increased depressive symptoms has been established, studies concede that this association may instead be due to contextual factors. Common risk factors like poor social or family dynamics and the use of other drugs have all been found to increase the risk of both depression and heavy marijuana use among people. It’s also possible that this association is dose-related and only applies to heavy users and cannabis-dependent individuals.

Data-driven care that works
Charlie Health’s virtual IOP delivers industry-leading clinical outcomes.
Associations between marijuana, depression and other factors
The relationship between marijuana, depression, and external life factors is certainly an intricate one; as mentioned, some research attributes marijuana use to increased depression, but other research suggests that external factors can increase the risk of both marijuana use and depression. One of the main schools of thought is that the relationship between marijuana and depression is demographically mediated, meaning there may be common social or environmental factors that not only increase the risk of marijuana use, but depression as well. For instance, after the death of a loved one, someone might become depressed and turn to weed to self-medicate. Alternatively, an individual could become ostracized in their community as a result of their weed use, leading to depression. In short, both marijuana use and depression have the potential to cause circumstances in life which may raise the risk of the other occurring.
Marijuana withdrawal’s impact on depression
Contrary to popular belief, people can suffer from what’s known as marijuana withdrawal syndrome. While the symptoms of weed withdrawal are not nearly as severe as withdrawal from other substances such as opiates or alcohol, it still has the potential to cause physical and psychological discomfort for those trying to quit. In fact, research conducted in 2022 found depressed mood to be one of the main symptoms of marijuana withdrawal. Since depressed mood is one of the primary symptoms of marijuana withdrawal it’s possible that many depressed individuals, especially those using weed to self-medicate, are discouraged from quitting for fear their depression will worsen.
Some other common symptoms of cannabis withdrawal include:
- Anxiety
- Increased anger or aggression
- Irritability
- Trouble sleeping
- Loss of appetite
Charlie Health data: Teens, depression, and marijuana
As part of an ongoing quality improvement study, here at Charlie Health we collect data from our clients using self-report surveys in order to follow client trends, produce publications, and to improve the quality of care that we provide to our clients. A sample was collected of approximately 3,700 teens and young adults who were admitted and discharged from Charlie Health between May 2022 and May 2023. Only individuals who completed an intake and discharge survey upon entering and leaving the program were included in this sample.
The majority of all clients screened positive for depression upon intake (73.3%; PHQ-9 score ≥ 10).
- 34.1% of all clients at Charlie Health reported using weed at least once 30 days prior to intake.
- 26.6% of all clients at Charlie Health reported using weed at least once 30 days prior to discharge.
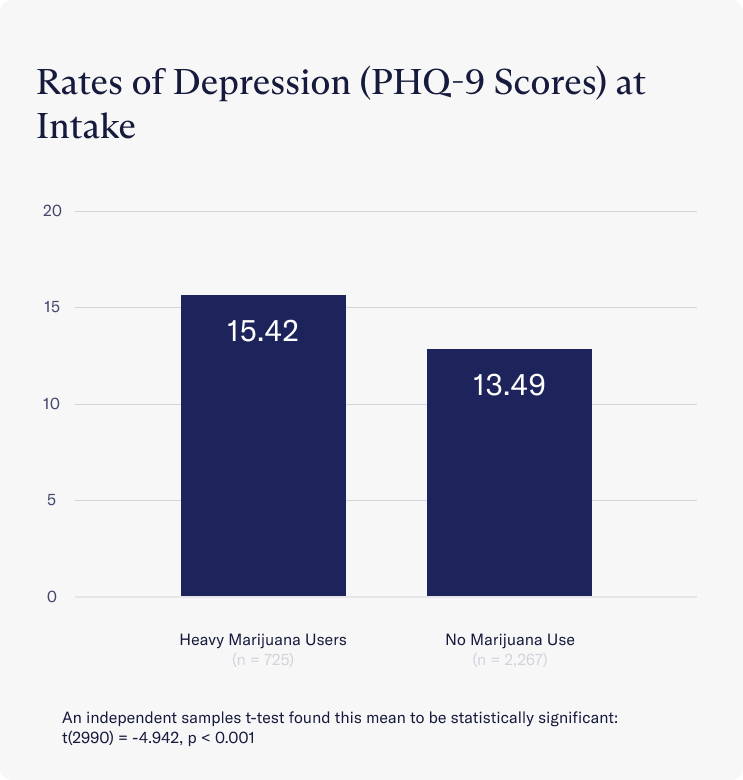
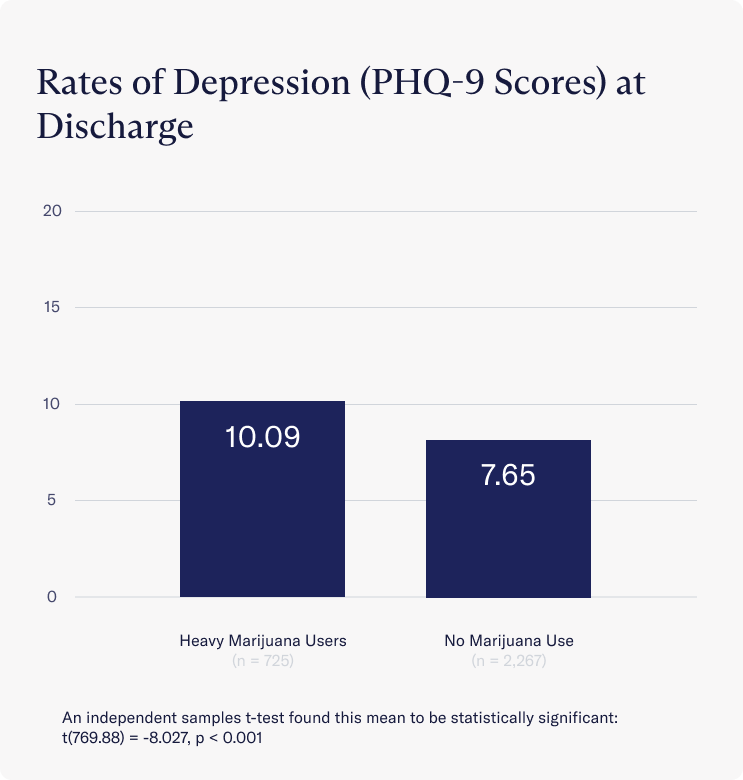
Rates of depressive symptoms among clients were measured using the Patient Health Questionnaire-9 scale for depression (PHQ-9), which categorizes depression into 5 groups ranging from “no depression” to “severe depression.” A significant difference emerged at both at intake and discharge in levels of depressive symptoms between clients who did not use marijuana and those who used it frequently.
Upon joining treatment at Charlie Health, clients who used marijuana frequently had significantly higher rates of depression on average than those who did not use marijuana. Those who used weed frequently were more likely to experience “moderately-severe” depressive symptoms (Avg = 15.42), while those who did not use marijuana experienced only “moderate” depressive symptoms on average (Avg = 13.49).
At discharge this trend continued but the differences in depressive symptoms between both groups became more pronounced. On average, clients who used marijuana frequently at discharge still met the clinical threshold for depression (Avg = 10.09), while those who abstained from marijuana no longer met this threshold (Avg = 7.65).
Three months after discharging from Charlie Health, clients who use marijuana frequently still presented with significantly higher rates of depressive symptoms than those who continued to abstain from marijuana. Those who abstained from marijuana use three months post-discharge remained below the clinical threshold for depression (Avg = 8.50), while frequent marijuana users on average remained clinically depressed (Avg = 11.21)
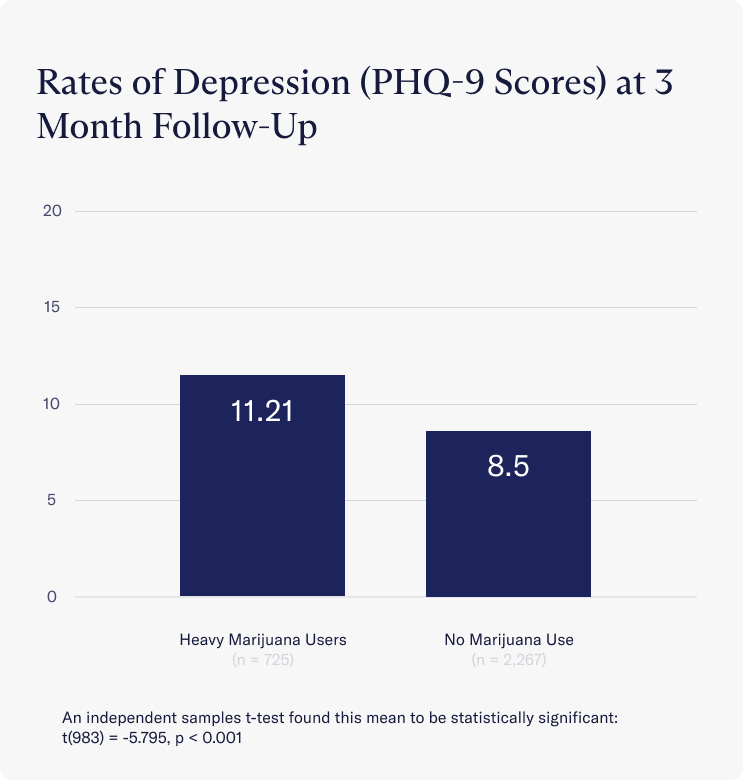
While this data doesn’t confirm that marijuana use increases depression, our findings at Charlie Health are consistent with current literature which has established an association between heavy marijuana use and increased depressive symptoms among individuals already struggling with depression.
Marijuana and depression: Our findings
Previous research has established an association between frequent marijuana use and increased depressive symptoms in individuals, especially among adolescents and young adults whose brains continue to develop into their mid-20s. As marijuana becomes increasingly accessible to children and teenagers across the United States, it’s important to understand the potential long term repercussions marijuana can have on young people who are still in these crucial stages of development. This is especially true for those who are at risk of or already have depression. In fact, research has shown individuals who begin using marijuana from a young age have a higher risk of developing a mental health issue such as depression later in life. While contemporary research has not confirmed a causal relationship between marijuana and depression, it’s important to understand the external and contextual factors that can increase the risk of both depression and heavy marijuana use.
Depression support at Charlie Health
Here at Charlie Health, our data seems to support previous research which found heavy marijuana users have higher rates of depression than those who do not use marijuana. While we cannot draw any concrete conclusions from these findings, other studies have determined that frequent marijuana use may exacerbate the symptoms of already existing depression and lead to overall poorer mental health in those struggling with mental health issues.
If you are struggling with depression and also use marijuana, you may want to consider abstaining from weed to optimize your recovery and improve your mental health. We’re here to help. Charlie Health’s virtual Intensive Outpatient Program (IOP) supports teens, young adults, and families who need more than once-weekly therapy. Our team of non-judgemental clinicians specialize in creating personalized care programs to manage a variety of mental health challenges, including depression. Fill out this short form and start healing today.
References
Connor, J. P., Stjepanović, D., Budney, A. J., Le Foll, B., & Hall, W. D. (2022). Clinical management of cannabis withdrawal. Addiction (Abingdon, England), 117(7), 2075–2095. https://doi.org/10.1111/add.15743
Recreational Cannabis Use By Teens Linked to Risk of Depression, Suicidality. (2023, May 5). Columbia University Department of Psychiatry. https://www.columbiapsychiatry.org/news/recreational-cannabis-use-among-u-s-adolescents-poses-risk-adverse-mental-health-and-life-outcomes
Osuch, E. A., Manning, K., Hegele, R. A., Théberge, J., Neufeld, R., Mitchell, D., Williamson, P., & Gardner, R. C. (2016). Depression, marijuana use and early-onset marijuana use conferred unique effects on neural connectivity and cognition. Acta Psychiatrica Scandinavica, 134(5), 399–409. https://doi.org/10.1111/acps.12629
Data and Statistics. (2022, April 22). https://www.cdc.gov/cannabis/data-research/facts-stats/
Grunberg, V. A., Cordova, K. A., Bidwell, L. C., & Ito, T. A. (2015). Can marijuana make it better? Prospective effects of marijuana and temperament on risk for anxiety and depression. Psychology of Addictive Behaviors, 29(3), 590–602. https://doi.org/10.1037/adb0000109
Langlois, C., Potvin, S., Khullar, A., & Tourjman, S. V. (2021). Down and High: Reflections Regarding Depression and Cannabis. Frontiers in Psychiatry, 12. https://doi.org/10.3389/fpsyt.2021.625158
Bahorik, A. L., Leibowitz, A., Sterling, S. A., Travis, A., Weisner, C., & Satre, D. D. (2017). Patterns of marijuana use among psychiatry patients with depression and its impact on recovery. Journal of Affective Disorders, 213, 168–171. https://doi.org/10.1016/j.jad.2017.02.016
Degenhardt, L., Hall, W., & Lynskey, M. (2003). Exploring the association between cannabis use and depression. Addiction, 98(11), 1493–1504. https://doi.org/10.1046/j.1360-0443.2003.00437.x
Hashemi, D., & Gray, K. (2023). Cannabis Use Disorder in Adolescents. Child and Adolescent Psychiatric Clinics of North America, 32(1), 13–20. https://pubmed.ncbi.nlm.nih.gov/36410900/




